15 Clinical guidelines now recommend vitamin D
Vitamin D recommendations in clinical guidelines: A systematic review, quality evaluation and analysis of potential predictors
Int J Clin Pract. 2021 Nov;75(11):e14805. doi: 10.1111/ijcp.14805. Epub 2021 Sep 15.
David Fraile Navarro 1 2 3, Alberto López García-Franco 1 2, Ena Niño de Guzmán 4, Montserrat Rabassa 4, Rocío Zamanillo Campos 5 6 7, Héctor Pardo-Hernández 8 9, Ignacio Ricci-Cabello 5 7 9, Carlos Canelo-Aybar 4, Jose F Meneses-Echavez 10 11, Juan José Yepes-Nuñez 12 13, Jesse Kuindersma 14, Ignasi Gich Saladich 4 9 15, Pablo Alonso-Coello 4 9
 OptimumOptimal Vitamin D level: 40, 50, 60, 70, 80 ng/mL? Controversy
OptimumOptimal Vitamin D level: 40, 50, 60, 70, 80 ng/mL? Controversy📄 Download the PDF from Sci-Hub via Vitamin D Life
Background: Vitamin D has been widely promoted for bone health through supplementation and fortification of the general adult population. However, there is growing evidence that does not support these strategies. Our aim is to review the quality and recommendations on vitamin D nutritional and clinical practice guidelines and to explore predictive factors for their direction and strength.
Methods: We searched three databases and two guideline repositories from 2010 onwards. We performed a descriptive analysis, a quality appraisal using AGREE II scores (Appraisal of Guidelines Research and Evaluation) and a bivariate analysis evaluating the association between direction and strength of recommendations, AGREE II domains' scores and pre-specified characteristics.
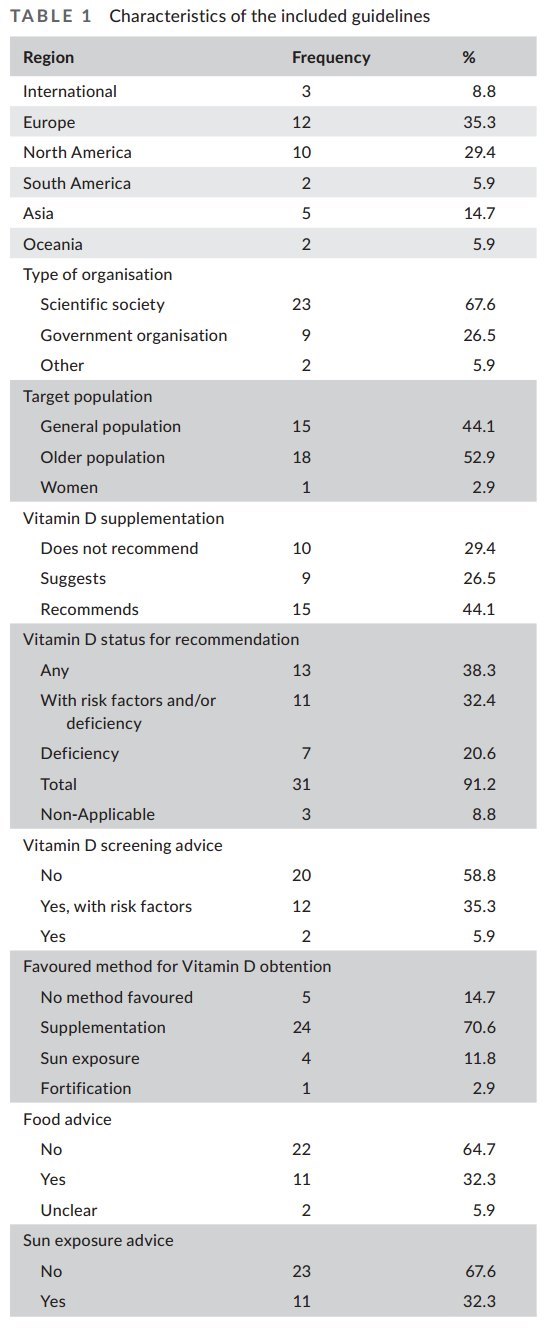
Results: We included 34 guidelines,
44.1% recommended,
26.5% suggested and
29.4% did not recommend vitamin D supplementation.
Guidelines that scored higher for "editorial independence" and "overall quality score" were less likely to recommend or suggest vitamin D supplementation (median 68.8 vs 35.4; P = .001 and 58.3 vs 37.5; P = .02). Guidance produced by government organisations and those that reported source of funding were associated with higher AGREE II scores. Unclear role of source of funding was associated with recommending or suggesting vitamin D supplementation (P = .034). Editorial independence was an independent predictor for recommending or suggesting vitamin D supplementation (OR 1.09; CI95% 1.02 to 1.16; P = .006).
Conclusions: Policymakers, clinicians and patients should be aware that lower quality guidelines and those reporting conflicts of interest are more likely to promote vitamin D supplementation. Guideline organisations should improve the quality of their recommendations' development and the management of conflicts of interest. Users and editors should be aware of these findings when using and appraising guidelines.
Clipped from PDF
Most CGs (33, 97.1%) targeted the elderly people,
22 (64.7%) targeted women,
18 (52.9%) targeted the general population and
seven (20.6%) targeted children.
Many extensive tables in the PDF, but many are two pages wide, so are difficult to put on the web