Washington EDU on Vitamin D
courses.washington.edu/bonephys/opvitD.html
Updated April 2010 Downloaded July 2010
Vitamin D requirements
There are three sources of vitamin D: natural sunlight, fortification of dietary foods, particularly dairy products and some cereals and oily fish. The radiation that converts vitamin D in the skin is the same wavelength that causes sunburn, so careful application of sunscreen can inhibit vitamin D production. At northern latitudes, there is not enough radiation to convert vitamin D, especially during the winter. After the age of 70 the skin does not convert vitamin D effectively (MacLaughlin J). Vitamin D levels depend on the pigmentation in the skin (darker skinned people have lower vitamin D levels), the altitude (higher levels in the mountains), and body weight (obese people have lower levels than thin people).
| Vitamin D supplementation | |
| People with poor sunlight exposure | 400-1000 units/day |
|---|---|
| Adults older than 70 | 800-1000 units/day |
| Patients with cystic fibrosis | 800-1000 units/day |
| Patients with malabsorption | Up to 50,000 units/day, check levels |
| Patients with liver disease | May need active metabolites |
| Patients with kidney disease | Need active metabolites |
| Patients with sarcoidosis or kidney stones | Be careful not to give excess Check levels, don't exceed 30 ng/mL |
Many vitamin D supplements also contain high contents of vitamin A - and recent studies show that vitamin A can increase bone resorption. The labels do not have to list the vitamin A, but it is often there, especially if it comes from cod liver oil.
Cholecalciferol is preferred because it sustains blood levels for a longer time (Armas, Glendenning P).
Vitamin D levels in serum
| 25 (OH) D Level | ng/ml (used in USA) | nMol/L (international) |
| Deficient | less than 8 | less than 20 |
|---|---|---|
| Insufficient | 8-20 | 20-50 |
| Optimal | 20-60 | 50-150 |
| High | 60-90 | 150-225 |
| Toxic | greater than 90 | greater than 225 |
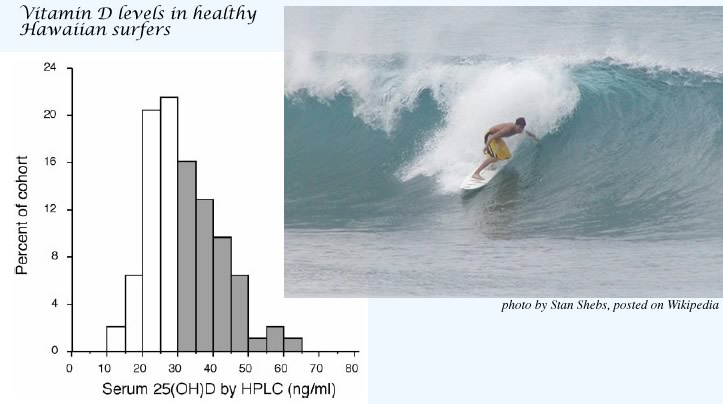
Binkley N, Low Vitamin D status despite abundant sun exposure.
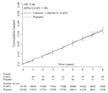
J Clin Endocrinol Metab 92:2130, 2007. copyright 2007, The Endocrine Society
The above graph shows results from 93 healthy 24-year-old Hawaiian surfers. The authors of this paper concluded that: "the goal of vitamin D replacement therapy should be no greater than the maximum that appears attainable, a serum 25(OH)D concentration of approximately 60 ng/ml." However, many laboratories currently have listed their "sufficient" range as 32-150 ng/ml. There is no evidence that levels above 60 ng/ml are beneficial.
There is disagreement about whether the lower limit of the optimal vitamin D levels should be 20 or 30 ng/ml, but none of the experts in the field still think that levels lower than 20 ng/ml are desirable. This is really different from ten years ago, when levels above 15 ng/dl were considered sufficient.
In another paper, Binkley N found differences among the laboratory tests for 25(OH) vitamin D of around 5 ng/dL, and approximately 10% error within the same lab. These errors must be taken into account when interpreting the vitamin D levels.
Vitamin D metabolism
Here is a little Flash slide show about vitamin D formation and actions:
ject width="610px" height="420px" align="middle" id="vitd" codebase="http://fpdownload.macromedia.com/pub/shockwave/cabs/flash/swflash.cab#version=7,0,0,0" classid="clsid:d27cdb6e-ae6d-11cf-96b8-444553540000">
bed width="610px" height="420px" align="middle" pluginspage="http://www.macromedia.com/go/getflashplayer" type="application/x-shockwave-flash" allowscriptaccess="sameDomain" name="vitd" bgcolor="#ffffff" quality="high" src="http://courses.washington.edu/bonephys/Gallery/vitd.swf"> 
Measure 25(OH) vitamin D, NOT 1,25(OH)2 vitamin D1,25(OH)2 vitamin D [1,25-D] is more difficult and expensive to measure than 25(OH)D; moreover, it is not a good measure of vitamin D status. When patients are vitamin D deficient, the parathyroid hormone increases and drives the renal 1-alpha-hydroxylase, so that 1,25-D levels increase. Only in severe deficiency, when substrate is depleted, does the 1,25-D become low. Partially treated vitamin D deficiency also results in marked elevations of 1,25-D levels. |
Vitamin D and Mortality
Melamed ML followed 13,331 adults in the US for 8.7 years to see if the vitamin D level was related to mortality. Notice that the mortality increases with either high or low levels of vitamin D (just like some of the other steroid hormones). 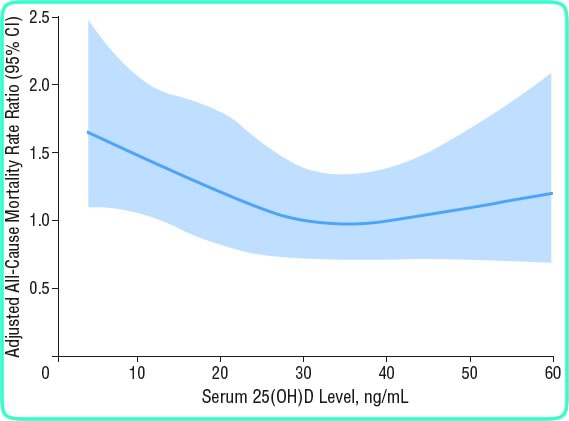
copyright American Medical Association, used with permission
Another study (Dobnig H) from Germany found lower mortality in people in the top 25% of vitamin D levels, compared to those with the lower 25%. The overall levels, however, were quite low; almost everybody was lower than 33 ng/ml.
 A meta-analysis of clinical trials of vitamin D (average dose was about 500 units/day) found an overall reduction in mortality of 7% (Autier P).
A meta-analysis of clinical trials of vitamin D (average dose was about 500 units/day) found an overall reduction in mortality of 7% (Autier P).
Click to enlarge this Forest Plot of mortality from randomized trials of vitamin D. Overall there was a non-significant decrease of 7% in the vitamin D groups compared to placebo (Chung) This report was sponsored by the US Agency for Healthcare Research and Quality.
Vitamin D and fractures
ject width="610px" height="420px" align="middle" id="vitd" codebase="http://fpdownload.macromedia.com/pub/shockwave/cabs/flash/swflash.cab#version=7,0,0,0" classid="clsid:d27cdb6e-ae6d-11cf-96b8-444553540000">
bed width="610px" height="420px" align="middle" pluginspage="http://www.macromedia.com/go/getflashplayer" type="application/x-shockwave-flash" allowscriptaccess="sameDomain" name="vitd" bgcolor="#F0F8FF" quality="high" src="http://courses.washington.edu/bonephys/Gallery/vitDfxrisk.swf">
Vitamin D and cancer
Vitamin D can suppress growth of cancer cells grown in culture. Therefore, researchers have tried to determine whether vitamin D levels are associated with cancer, and whether vitamin D could be used to prevent or treat cancer. Early studies were promising, but recent larger studies do not find the same encouraging results. Click to see recent large prospective observational studies relating vitamin D to colon, breast, or prostate cancer: ject width="520" height="450" align="middle" id="vitDcancer" codebase="http://download.macromedia.com/pub/shockwave/cabs/flash/swflash.cab#version=10,0,0,0" classid="clsid:d27cdb6e-ae6d-11cf-96b8-444553540000">bed width="520" height="450" align="middle" pluginspage="http://www.adobe.com/go/getflashplayer" type="application/x-shockwave-flash" allowfullscreen="false" allowscriptaccess="sameDomain" name="vitDcancer" bgcolor="#ffffff" quality="high" src="http://courses.washington.edu/bonephys/Gallery/vitDcancer.swf">
Colon cancer
 Vitamin D probably protects against colon cancer (Wei MY, Giovannucci E,Freedman DM). Click to enlarge this Forest Plot of colon cancer from studies of vitamin D. (Chung) This report was sponsored by the US Agency for Healthcare Research and Quality. Since then, a large nested case-control study in Europe found an increased risk in men with low vitamin D (Jenab M; results are shown on the image above). Another study looking at different ethnic groups also found lower risk of those in the lowest quintile of vitamin D (less than 16.8 ng/ml), but no difference in the other 80% of patients (Woolcott CG).
Vitamin D probably protects against colon cancer (Wei MY, Giovannucci E,Freedman DM). Click to enlarge this Forest Plot of colon cancer from studies of vitamin D. (Chung) This report was sponsored by the US Agency for Healthcare Research and Quality. Since then, a large nested case-control study in Europe found an increased risk in men with low vitamin D (Jenab M; results are shown on the image above). Another study looking at different ethnic groups also found lower risk of those in the lowest quintile of vitamin D (less than 16.8 ng/ml), but no difference in the other 80% of patients (Woolcott CG).
Breast Cancer
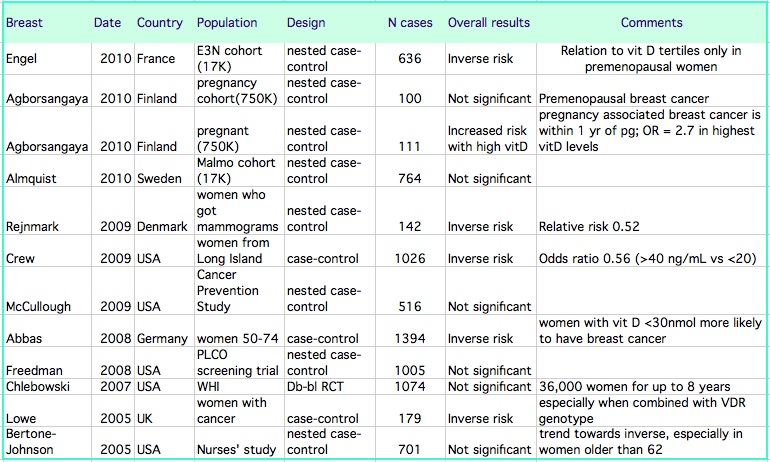
( Abbas S, Agborsangaya CB, Almquist M, Bertone-Johnson ER, Freedman DM, McCullough ML)
 In the Women's Health Initiative randomized clinical trial of calcium and vitamin D, which included 36,000 women, there was no difference in the incidence of breast cancer between those assigned to placebo or to calcium and vitamin D (Chlebowski RT). Click on the thumbnail to enlarge the graph from that study. However, if the intake of vitamin D included the supplements taken by the subjects, then those with the highest intakes had higher risk of breast cancer.
In the Women's Health Initiative randomized clinical trial of calcium and vitamin D, which included 36,000 women, there was no difference in the incidence of breast cancer between those assigned to placebo or to calcium and vitamin D (Chlebowski RT). Click on the thumbnail to enlarge the graph from that study. However, if the intake of vitamin D included the supplements taken by the subjects, then those with the highest intakes had higher risk of breast cancer.
Prostate Cancer
 Early studies suggested the men with low vitamin D levels were more likely to get prostate cancer, but newer, larger studies do not find this. Click to enlarge this Forest Plot of prostate cancer from studies of vitamin D. (Chung) This report was sponsored by the US Agency for Healthcare Research and Quality. In the large Prostate, Lung, Colorectal and ovarian cancer screening trial (PLCO), the risk of aggressive prostate cancer was higher in men with higher vitamin D levels, as shown in the colored graph above (Ahn J). Two newer studies within the last year continue to show no significant benefit of vitamin D - one was a case control study of men with different ethnicities, including 329 cases (Park SY) and the other a large nested case control study from the European Prospective Investigation into Cancer and Nutrition (EPIC) study, which included 652 cases ( Travis RC).
Early studies suggested the men with low vitamin D levels were more likely to get prostate cancer, but newer, larger studies do not find this. Click to enlarge this Forest Plot of prostate cancer from studies of vitamin D. (Chung) This report was sponsored by the US Agency for Healthcare Research and Quality. In the large Prostate, Lung, Colorectal and ovarian cancer screening trial (PLCO), the risk of aggressive prostate cancer was higher in men with higher vitamin D levels, as shown in the colored graph above (Ahn J). Two newer studies within the last year continue to show no significant benefit of vitamin D - one was a case control study of men with different ethnicities, including 329 cases (Park SY) and the other a large nested case control study from the European Prospective Investigation into Cancer and Nutrition (EPIC) study, which included 652 cases ( Travis RC).