Recurrent pre term birth and low vitamin D
Vitamin D status and recurrent preterm birth: a nested case-control study in high-risk women.
BJOG. 2012 Dec;119(13):1617-23. doi: 10.1111/j.1471-0528.2012.03495.x. Epub 2012 Oct 19.
Thorp JM, Camargo CA, McGee PL, Harper M, Klebanoff MA, Sorokin Y, Varner MW, Wapner RJ, Caritis SN, Iams JD, Carpenter MW, Peaceman AM, Mercer BM, Sciscione A, Rouse DJ, Ramin SM, Anderson GB; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network.
Collaborators (61)
Department of Obstetrics and Gynecology, University of North Carolina School of Medicine, Chapel Hill, NC 27599-7570, USA. [email protected]
OBJECTIVE: To determine whether vitamin D status is associated with recurrent preterm birth, and any interactions between vitamin D levels and fish consumption.
DESIGN: A nested case-control study, using data from a randomised trial of omega-3 fatty acid supplementation to prevent recurrent preterm birth.
SETTING: Fourteen academic health centres in the USA.
POPULATION: Women with prior spontaneous preterm birth.
METHODS: In 131 cases (preterm delivery at <35 weeks of gestation) and 134 term controls, we measured serum 25-hydroxyvitamin D [25(OH)D] concentrations by liquid chromatography-tandem mass spectrometry (LC-MS) from samples collected at baseline (16-22 weeks of gestation). Logistic regression models controlled for study centre, maternal age, race/ethnicity, number of prior preterm deliveries, smoking status, body mass index, and treatment.
MAIN OUTCOME MEASURES: Recurrent preterm birth at <37 and <32 weeks of gestation.
RESULTS: The median mid-gestation serum 25(OH)D concentration was 67 nmol/l, and 27% had concentrations of <50 nmol/l. Serum 25(OH)D concentration was not significantly associated with preterm birth (OR 1.33; 95% CI 0.48-3.70 for lowest versus highest quartiles). Likewise, comparing women with 25(OH)D concentrations of 50 nmol/l, or higher, with those with <50 nmol/l generated an odds ratio of 0.80 (95% CI 0.38-1.69). Contrary to our expectation, a negative correlation was observed between fish consumption and serum 25(OH)D concentration (-0.18, P < 0.01).
CONCLUSIONS: In a cohort of women with a prior preterm birth, vitamin D status at mid-pregnancy was not associated with recurrent preterm birth.
© Published 2012. This article is a U.S. Government work and is in the public domain in the USA. © 2012 RCOG.
PMID: 23078336
PDF is attached at the bottom of this page
Observation by Vitamin D Life
This study excluded women with histories of pre-eclampsia (another pathway to early delivery), a condition that is most often linked to low vitamin D status.
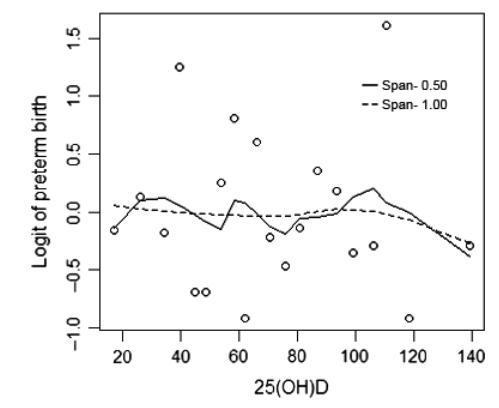
Wonder if the data circles of 20 women each which show very high recurrent pre-term birth are associated with the women who did not get Omega-3 supplements
The data on the chart has a lot of variance.
- There are very few data points data at the average, most of the data clusters are far above or far below the average.
