Vitamin D prescribing in children in UK primary care practices: a population-based cohort study
Paediatrics http://dx.doi.org/10.1136/bmjopen-2019-031870
Mandy Wan1,2, Laura J Horsfall3, Emre Basatemur4, Jignesh Prakash Patel2,5, Rukshana Shroff6, Greta Rait3
Still a long ways to go - it appears that only 3% of youths now have Vitamin D prescriptions
Increased use of D category listing has 38 items including the following- Vitamin D use increased 3.7 X, Omega-3 increased 9 X (US 1999-2012) – JAMA Oct 2016
- Vitamin D levels increasing 7 percent per year, bones denser in Japan (probably supplementation) - June 2015
- Vitamin D supplementation in Ireland - big increase in people with 20-50 nanograms in 20 years – June 2015
- Vitamin D in US children: those having more than 40 ng increased 60 percent (2001-2010) - Dec 2016
- Vitamin D overtakes Vitamin C to become the UK's best-selling supplement – Jan 2019
- People are not limited to prescriptions in England - it is so low cost they can just buy it
- 4 times fewer with vitamin D deficiency in just 4 years ( Connecticut) – March 2016
- 20X increase in vitamin D sold and 36 percent decrease in osteoporosis business in Australia – Nov 2013
Download the PDF from Vitamin D Life

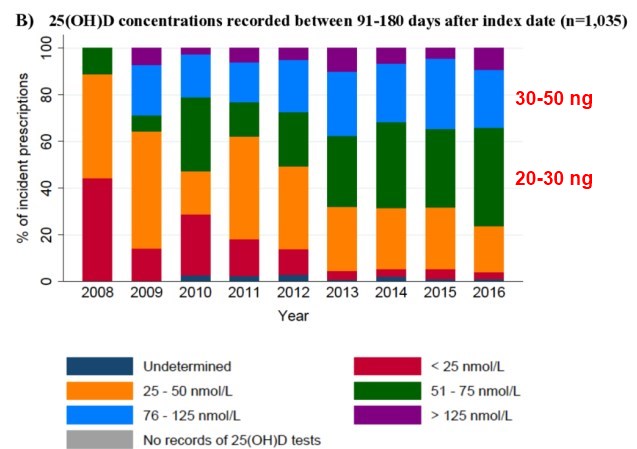
Vitamin D Levels After 6 months
Objective To examine temporal changes in the incidence and patterns of vitamin D supplementation prescribing by general practitioners (GPs) between 2008 and 2016.
Design Population-based cohort study.
Setting UK general practice health records from The Health Improvement Network.
Participants Children aged 0 to 17 years who were registered with their general practices for at least 3 months.
Outcome measures Annual incidence rates of vitamin D prescriptions were calculated, and rate ratios were estimated using multivariable Poisson regression to explore differences by sociodemographic factors. Data on the type of supplementation, dose, dosing schedule, linked 25-hydroxyvitamin D (25(OH)D) laboratory test results and clinical symptoms suggestive of vitamin D deficiency were analysed.
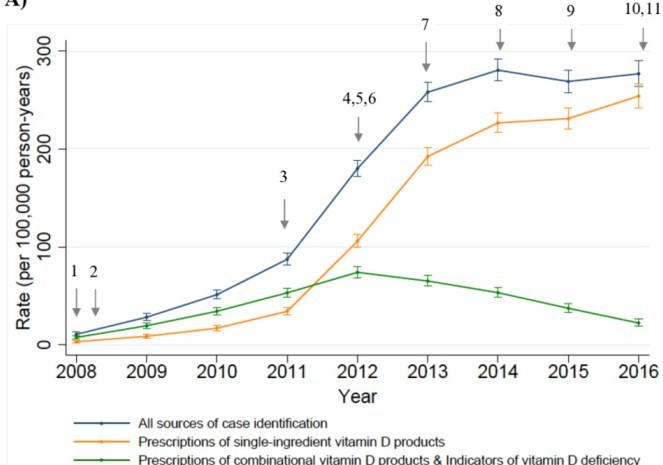
Results Among 2 million children, the crude annual incidence of vitamin D prescribing increased by 26-fold between 2008 and 2016 rising from 10.8 (95% CI: 8.9 to 13.1) to 276.8 (95% CI: 264.3 to 289.9) per 100 000 person-years. Older children, non-white ethnicity and general practices in England (compared with Wales/Scotland/Northern Ireland) were independently associated with higher rates of prescribing. Analyses of incident prescriptions showed inconsistent supplementation regimens with an absence of pre-supplementation 25(OH)D concentrations in 28.7% to 56.4% of prescriptions annually. There was an increasing trend in prescribing at pharmacological doses irrespective of 25(OH)D concentrations, deviating in part from UK recommendations. Prescribing at pharmacological doses for children with deficient status increased from 3.8% to 79.4%, but the rise was also observed in children for whom guidelines recommended prevention doses (0% to 53%). Vitamin D supplementation at pharmacological doses was also prescribed in at least 40% of children with no pre-supplementation 25(OH)D concentrations annually.
Conclusions There has been a marked and sustained increase in vitamin D supplementation prescribing in children in UK primary care. Our data suggests that national guidelines on vitamin D supplementation for children are not consistently followed by GPs.
26 X increase in Vitamin D prescriptions for youths in England in 8 years – Dec 2019 505 visitors, last modified 16 Dec, 2019,
Printer Friendly PDF this page! Follow this page for updates This page is in the following categories (# of items in each category) Youth 148 Vitamin D in Europe 208 Infant-Child 606 Increased use of D 38 Attached files
ID Name Comment Uploaded Size Downloads 13096 England 6 month.jpg admin 05 Dec, 2019 02:56 52.25 Kb 122 13095 England 12-17.jpg admin 05 Dec, 2019 02:55 62.06 Kb 147 13094 England A.jpg admin 05 Dec, 2019 02:55 44.94 Kb 139 13093 England 26X.pdf admin 05 Dec, 2019 02:54 858.70 Kb 171
See any problem with this page? Report it (FINALLY WORKS)
- Vitamin D use increased 3.7 X, Omega-3 increased 9 X (US 1999-2012) – JAMA Oct 2016
- Vitamin D levels increasing 7 percent per year, bones denser in Japan (probably supplementation) - June 2015
- Vitamin D supplementation in Ireland - big increase in people with 20-50 nanograms in 20 years – June 2015
- Vitamin D in US children: those having more than 40 ng increased 60 percent (2001-2010) - Dec 2016
- Vitamin D overtakes Vitamin C to become the UK's best-selling supplement – Jan 2019
- People are not limited to prescriptions in England - it is so low cost they can just buy it
- 4 times fewer with vitamin D deficiency in just 4 years ( Connecticut) – March 2016
- 20X increase in vitamin D sold and 36 percent decrease in osteoporosis business in Australia – Nov 2013
Download the PDF from Vitamin D Life
Vitamin D Levels After 6 months
Objective To examine temporal changes in the incidence and patterns of vitamin D supplementation prescribing by general practitioners (GPs) between 2008 and 2016.
Design Population-based cohort study.
Setting UK general practice health records from The Health Improvement Network.
Participants Children aged 0 to 17 years who were registered with their general practices for at least 3 months.
Outcome measures Annual incidence rates of vitamin D prescriptions were calculated, and rate ratios were estimated using multivariable Poisson regression to explore differences by sociodemographic factors. Data on the type of supplementation, dose, dosing schedule, linked 25-hydroxyvitamin D (25(OH)D) laboratory test results and clinical symptoms suggestive of vitamin D deficiency were analysed.
Results Among 2 million children, the crude annual incidence of vitamin D prescribing increased by 26-fold between 2008 and 2016 rising from 10.8 (95% CI: 8.9 to 13.1) to 276.8 (95% CI: 264.3 to 289.9) per 100 000 person-years. Older children, non-white ethnicity and general practices in England (compared with Wales/Scotland/Northern Ireland) were independently associated with higher rates of prescribing. Analyses of incident prescriptions showed inconsistent supplementation regimens with an absence of pre-supplementation 25(OH)D concentrations in 28.7% to 56.4% of prescriptions annually. There was an increasing trend in prescribing at pharmacological doses irrespective of 25(OH)D concentrations, deviating in part from UK recommendations. Prescribing at pharmacological doses for children with deficient status increased from 3.8% to 79.4%, but the rise was also observed in children for whom guidelines recommended prevention doses (0% to 53%). Vitamin D supplementation at pharmacological doses was also prescribed in at least 40% of children with no pre-supplementation 25(OH)D concentrations annually.
Conclusions There has been a marked and sustained increase in vitamin D supplementation prescribing in children in UK primary care. Our data suggests that national guidelines on vitamin D supplementation for children are not consistently followed by GPs.
| 505 visitors, last modified 16 Dec, 2019, |
| ID | Name | Comment | Uploaded | Size | Downloads | |
|---|---|---|---|---|---|---|
| 13096 | England 6 month.jpg | admin 05 Dec, 2019 02:56 | 52.25 Kb | 122 | ||
| 13095 | England 12-17.jpg | admin 05 Dec, 2019 02:55 | 62.06 Kb | 147 | ||
| 13094 | England A.jpg | admin 05 Dec, 2019 02:55 | 44.94 Kb | 139 | ||
| 13093 | England 26X.pdf | admin 05 Dec, 2019 02:54 | 858.70 Kb | 171 |
