Vitamin D non-skeletal trials – review
Results of Vitamin D RCTs with Beneficial Non-Skeletal Effects,
Those that Failed, and
Expectations for those Underway
William B. Grant, Ph.D.
Sunlight, Nutrition and Health Research Center (SUNARC), San Francisco, CA 94164-1603, [email protected], www.sunarc.org
SUNARC receives funding from Bio-Tech Pharmacal (Fayetteville, AR), The UV Foundation, and The Sunlight Research Forum (Veldhoven).
Poster presented at Vitamin D Workshop in Chicago, June 2014
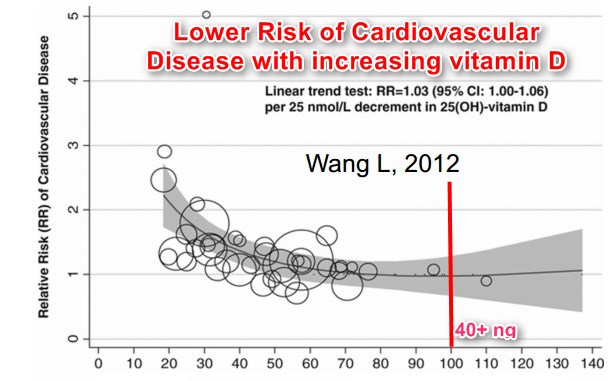
Figure 1 CVD risk vs Vitamin D level
red text and lines were added by Vitamin D Life
Background:
A number of recent papers have pointed out that most vitamin D randomized controlled trials (RCTs) to date have not found beneficial effects when conducted on healthy populations in Western developed countries. There could be several reasons for these general failures. One is that vitamin D may not affect risk of disease. A second is that too little vitamin D was used in the trials. A third is that serum 25-hydroxyvitamin D [25(OH)D] levels were too high to show an effect for the vitamin D doses used in the studies.
Materials and methods:
A literature search was conducted at pubmed.gov for vitamin D RCTs finding beneficial effects for non-skeletal outcomes. Studies that used combined vitamin D plus calcium were generally excluded unless there was also a calcium-only arm. In addition, data from large unsuccessful vitamin D RCTs were obtained, as well as the designs of the five major vitamin D RCTs underway on adults. 25(OH)D levels for the various studies were estimated based on 25(OH)D levels for the populations from which the participants were drawn.
Results:
21 vitamin D RCTs with beneficial effects for non-skeletal outcomes were identified. The aims, conditions, and results for these studies were tabulated. The successful vitamin D RCTs tended to be conducted on populations with low 25(OH)D levels (<50 nmol/L) and with 1000-4000 IU/d vitamin D3. The unsuccessful vitamin D RCTs were conducted on populations with 25(OH)D levels between 50 and 65 nmol/L and used 400-2800 IU/d. The major vitamin D RCTs underway are being conducted on populations with 25(OH)D levels between 40 and 75 nmol/L and are using 1600 to 3330 IU/d vitamin D3.
Discussion:
The lower the 25(OH)D level of the participants and the higher the vitamin D dose, the greater likelihood of finding significant beneficial nonskeletal effects. Some of the major vitamin D RCTs underway should find significant beneficial effects for cancer, cardiovascular disease, and other nonskeletal effects, but others may not. The outcomes will depend on the baseline 25(OH)D levels of the participants and the extent to which vitamin D affects the major health outcomes such as cancer and cardiovascular disease.
Conclusion:
The failure of vitamin D RCTs to confirm the findings of ecological and observational studies to date should not be considered evidence that vitamin D does not have beneficial effects but, rather, the result of poor design of the vitamin D RCTs.
Successful vitamin D RCTs
The populations from which the participants in the successful vitamin D RCTs were drawn include African-Americans, those living in Argentina, Iran, Mongolia, and Turkey, those with COPD, diabetes mellitus, PCOS, prostate cancer, or who are obese, and those taking statins. Trial durations ranged from two months to four years. The number of participants in the trials, including those in all arms, ranged from 8 to 1179. Evidently large numbers of participants are not required for significant effects if the serum 25(OH)D levels are low enough, the vitamin D doses high enough, and the population at increased risk of the health outcomes.
Caveats regarding vitamin D RCTs
One thing vitamin D RCTs cannot assess is the effect of 25(OH)D levels prior to the age of the participants. There is increasing evidence that there are important in utero effects on risk of breast cancer as an adult, for example. A classic example of the effect of early life environmental influences on cancer risk is the multicountry ecological study of diet and risk of cancer that identified animal fat and animal protein as important risk factors for cancers common in Western developed countries [Armstrong and Doll, 1975]. The results of this study were disputed for years until Harvard was able to confirm that meat was a risk factor for breast cancer in younger women [Cho, 2006]. The results of the 1975 study were largely confirmed in a more recent study [Grant, 2014]. Thus, vitamin D RCTs may have a harder time confirming ecological studies based on geographical variations of solar UVB doses than in confirming observational studies based on 25(OH)D levels.
Another caveat is that some of the associations between solar UVB doses and serum 25(OH)D levels and health outcomes may be due to UV effects of both vitamin D and other, as yet undetermined mechanisms. See the recent paper by Rebel et al. [2014], which found in a mouse model that UV irradiance had a larger impact on intestinal cancer than oral vitamin D, even though both approaches increased 25(OH)D levels the same amount.
Table 1. Successful vitamin D RCTs - non-skeletal effects
Reference | Aims: Investigate the effect of vitamin D supplementation on | Population | Study period | Intervention (vitamin D3 unless otherwise noted) (IU) | Initial, final 25(OH) level (nmol/L) | Key findings | |
Aloia, 2007 | Risk of colds and influenza | 208 African-American postmenopausal women in Long Island, NY | 3 yrs | 800/d for 2 yrs (n = 104) followed by 2000/d for 1 yr or placebo | 47±29; 87±27 | 30 colds or influenza for placebo, 8 for 800 IU/d, 1 for 2000 IU/d | |
Lappe, 2007 | Risk of cancer | 1179 women >55 yrs in Nebraska | Years 24 of 4-yr study | 1450 mg calcium or 1450 mg calcium plus 1100/d | 72±20 96±21 | RRfor the Ca_D group 0.23 (CI: 0.09, 0.60; P = 0.005). RR for the Ca-only group, RR= 0.59 (0.29, 1.21; P = 0.15). | |
Zittermann, 2009 | CVD risk factors | 163 obese (BMI = 33.7± 4.1 kg/m2) men and women aged 48±10 yrs | 12 mos | 3320/d | 30.0±17.5 85.5± 57.5 | triglycerides (-13.5% compared with +3.0%; P < 0.001), and the inflammation marker tumor necrosis factor-alpha (-10.2% compared with -3.2%; P = 0.049) | |
Dong, 2010 | Arterial stiffness measured by PWV | 49 African-Americans aged 16.3±1.4 yrs in Agusta, GA | 16 wks | 2000/d | 34.0±10.6 59.8±18.2 | PWV in cases 5.41 ±0.73 to 5.33±0.79 m/s Vs. controls 5.38±0.53 to 5.71±0.75 m/s (p=0.03) | |
Selimoglu, 2010 | Glucose metabolism, insulin, and androgen levels in obese, insulin-resistant women with PCOS | 11 women with PCOS, 23.6±5.7 yr, body mass index 33.9±5.1 kg/m2, Turkey | 300,000 once | 42.3±40 92.8±36.5 | (HOMA)-IR significantly decreased from 4.41±1.38 to 3.67±1.48 (p: 0.04) | ||
Urashima, 2010 | Incidence of influenza | 334 students in Japan; 280 of whom had not been taking vitamin D prior to the study | 4 mos | 1200/d | For those not taking supplements prior to the study, incidence of type a influenza (RR: 0.36; 95% CI: 0.17, 0.79; P = 0.006) | ||
Bock, 2011 | Regulatory T-cell numbers | 59 healthy adults in Austria | 3 mos | 140,000/mo | % peripheral regulatory T cells increased significantly in the vitD group, but remained unchanged in the placebo | ||
Harris, 2011 | Brachial artery flow-mediated dilation | 57 African-Americans aged 29±2 yrs, BMI = 30±2 kg/m2 in Agusta, GA | 16 wks | 60,000/mo | 34.3±2.2 100.9±6.6 | * 1.8±1.3% for treatment vs. -1.3±0.6% for placebo | |
Pilz, 2011 | Testosterone | 54 non-diabetic men in Austria or Germany | 1 yr | 3332/d | <50 Increased by 53.5 | total testosterone levels (from 10.7 ± 3.9 nmol/l to 13.4 ± 4.7 nmol/l; p < 0.001), bioactive testosterone (from 5.21 ± 1.87 nmol/l to 6.25 ± 2.01 nmol/l; p = 0.001), and free testosterone levels (from 0.222 ± 0.080 nmol/l to 0.267 ± 0.087 nmol/l; p = 0.001) | |
Camargo, 2012 | Acute respiratory infections | 247 Mongolian school children | Milk with or without 300/d vitamin D3 | 17.5 (12.525.0) 47.5 | RR = 0.50 [95% confidence interval: 0.28-0.88] | ||
Lehouck, 2012 | COPD exacerbations | 182 patients with moderate to very severe COPD and a history of recent exacerbations in Belgium | 1 yr | 100,000/4 wks | <25 Increased by 75 | reduction in exacerbations in the vitamin D group (rate ratio, 0.57 [CI, 0.33 to 0.98]; P = 0.04 | |
Marshall, 2012 | Prostate cancer progression | 44 men with low-grade prostate cancer in S. Carolina | 1 yr | 4000/d | 82±33 165±36 | 24 of 44 subjects (55%) showed a decrease in the number of positive cores or decrease in Gleason score; five subjects (11%) showed no change; 15 subjects (34%) showed an increase in the number of positive cores or Gleason score. | |
Salehpour, 2012a | Decrease in body fat | 77 women (age 38 ± 8.1 years, BMI 29.8 ± 4.1 kg/m2) in Iran | 12 wks | 1000/d | 37±30 Increase = 38.2 ± 32.7 vs. 4.6 ± 14.8; P<0.001 | Decrease in body fat (-2.7 ± 2.1 kg vs. -0.47 ± 2.1 kg; P<0.001). | |
Salehpour, 2012b | Risk of CVD | 77 women (age 38 ± 8.1 years, BMI 29.8 ± 4.1 kg/m2) in Iran | 12 wks | 1000/d | 37±30 Increase = 38.2 ± 32.7 vs. 4.6 ± 14.8; P<0.001 | mean HDL-cholesterol concentration increased, (0 07 (sd 0 2) v. - 0 03 (sd 0 2) mmol/l; P = 0 037). Mean apoA-I concentration increased (0 04 (sd 0 39) v. - 0 25 (sd 0 2) g/l; P < 0 001). Mean LDL-cholesterol:apoB-100 ratio augmented p (011 (sd 0 6) v. -019 (sd 03); P = 0014). | |
Belenchia, 2013 | HOMA-IR | 35 obese adolescent patients [age: 14.1 ± 2.8 y; BMI ( kg/m(2)): 39.8 ± 6.1] in Missouri | 6 mos | 4000/d | 49.0±17.8 Increase 48.8 vs. 7.0 for the placebo arm | HOMA-IR (-1.363 compared with +0.27 for placebo; P = 0.033), | |
Hossein- Nezhad, 2013 | Gene expression | 8 healthy adults in Boston in winter | 2 mos | 400/d (n-=3) or 2000/d (n=5) | 40.5±9.5 or 69.0±13.5; Increase = 14.0 or 24.5 | Change in expression of 113 genes, baseline and dose dependent | |
Rahimi- Ardabili, 2013 | CVD risk factors | 24 women aged 2030 yrs with PCOS in Iran | 2 mos | 150,000/20 d | 17.3±7.0 58.5±15.4 | TC from 196.5 to 179.0 mg/dL (p=0.049) TG from 156.8 to 130.5 mg/dL (p=0.053) VLDL from 31.9 ro 26.1 mg/dL (p=0.053). No change in serum HDLC, LDLC, APO-AI, and hs-CRP concentrations | |
Soheilykh ah, 2013 | HOMA-IR | 120 women with a gestational age of less than 12 weeks in Iran | 24 wks | 200/d, 50,000/mo, or 50,000/2 wks | 18.3±13.3, 68.0±26.8; 18.3±14.8, 85.3±28.8 | Insulin from 7.37 to 12.21 (p=0.001); HOMA-IR from 1.44 to 2.39 (p=0.001). Insulin from 8.0 to 11.6 (p=0.001); HOMA-IR from 1.54 to 2.24 (p=0.001) | |
Wagner, 2013 | Health characteristics and outcomes from pregnancy | 504 pregnant women, starting in 12th week | 24 wks | 2000/d, 4000/d | 60 77, 93, 105 | Combined morbidity OR per 25 nmol/L = 0.84 (0.74-0.95), p = 0.006 | |
Hirschler, 2014 | Cholesterol | 60 indigenous children, aged 9 yrs in Argentina | 2 mos | 100,000/mo | 36.8±12.9 80.4±20.7 | HDL, 39.9 to 43.9 (p<0.01) | |
Nasri, 2014 | Blood pressure | 60 type 2 diabetes patients aged 55 (sd=11) yrs in Iran | 12 wks | 50,000/wk | 84 (sd = 49-54) 163 (sd = 32-67) | Systolic BP from 121 (SD=13) mm to 110 (SD=9) mm, p=0.001 Diastolic BP from 80.5 (SD=8) mm to 76.3 (sd=7) mm, p=0.046 | |
Qin, 2014 | Cholesterol | 56 men and women aged 68±9 years taking statins in China | 6 mos | 2000 | 52.8±29.3 95.5±28.3 | LDL, 120±30 to 98±2 mg/dL (p=0.01); HDL, 43±13 to 51±12 mg/dL (p=0.01); TG, 111±62 to 79±35, p=0.03 | |
Reference | Aims " Investigate the effect of vitamin D supplementation on" | Population | Study period | Intervention (vitamin D3 unless otherwise noted) | Initial, final 25(OH) level (nmol/L) for interventio n arm | Key findings | |
Table 2. Results of vitamin D randomized controlled trials with no significant beneficial effects for non-skeletal effects
Reference | Aims: Investigate the effect of vitamin D supplementation on | Population | Study period | Intervention (vitamin D3 unless otherwise noted) (IU) | Initial, final 25(OH) level (nmol/L) | Key findings |
Trivedi, 2003 | Cancer, CVD incidence, mortality | 2686 women aged 65-85 yrs | 5 yrs | 100,000/4 mos | 53.4 (sd 21.1) 74.3 (sd 20.7) | RR for mortality 0.88 (0.74-1.06), p = 0.18 |
WHI, 2006 | Colorectal cancer | 36,282 women | 400 plus 1000 mg/d calcium | 70? | No significant results unless were not taking vitamin D or calcium prior to enrollment | |
Li-Ng, 2009 | Influenza | 162 African-American adults | 12 wks | 2000 | 64.3 (25.4) 88.5 (233.2) | No significant effect |
Jorde, 2010 | glucose tolerance, blood pressure or serum lipids | A total of 438 overweight or obese subjects, 21-70 years old, were included and 330 completed the study. | 1 yr | 20,000/wk 40,000/wk placebo | 58.4 ± 20.4 101 or 140 | No significant effects on OGIT, HbA1c, HOMA, or QUICKI |
Mitri, 2011 | pancreatic b cell function, insulin sensitivity, and glycemia | 92 adults at high risk of diabetes | 16 wks | 2000, some with 800 mg/d calcium | 60±7 | improvement in insulin secretion (62 6 39 compared with 236 6 37 mU • L21 • min, respectively; P = 0.046). Hb A1c increased less, but nonsignificantly, in the vitamin D group than in the no-vitamin D group (0.06 6 0.03% compared with 0.14 6 0.03%, respectively; P = 0.081). |
Avanell, 2012 | Cancer incidence, cancer or vascular mortality | 5292 people (85% women) aged at least 70 yr (mean age = 77 yrs) with previous low trauma fracture, UK, enrolled 1999-2002 | Mean follow-up 6.2 yrs | daily vitaminD3 (800 IU), calcium (1000 mg), both, or placebo for 2462 months, | 45 (Llewellyn, 2009) | hazard ratio (HR) =0.93 (0.85-1.02], vascular disease mortality HR = 0.91 (0.79-1.05), cancer mortality HR = 0.85 (0.68-1.06), and cancer incidence HR = 1.07 (0.92-1.25) |
Murdoch, 2012 | Upper respiratory tract infections | 322 healthy adults in Christchurch, New Zealand. | 18 mos | initial dose of 200 000 IU oral vitamin D3,, then 100 000 IU monthly | 72.5 >120 | risk ratio, 0.97 (0.85-1.11) |
Proper design of vitamin D RCTs
Several recent papers outlined why vitamin D RCTs often fail and how they should be designed for optimal expectation of success [Lappe, 2012; Heaney, 2014; Grant, 2014]. Most vitamin D RCTs are designed based on the model for trials of pharmaceutical drugs, i.e., the trial supplies the only source of the material and there is a linear dose-response relation. Neither assumption is valid for vitamin D. Thus, most vitamin D RCTs were designed to fail. Heaney [2014] outlined how vitamin D RCTs should be designed. First, they should start with an estimate of the 25(OH)D level-health outcome relation, generally from observational studies (see, also, Grant [2014]). Next, 25(OH)D levels of prospective participants should be obtained and only those with low 25(OH)D levels should be included in the study. The vitamin D dose should be large enough to raise 25(OH)D levels to the upper end of the quasi-linear region of the relation. 25(OH)D levels should be remeasured to ascertain compliance, often at about 80%, and to see whether the dose was sufficient. In addition, cofactors should be optimized. Designing and conducting vitamin D RCTs in this manner will enable the 25(OH)D level-health outcome relations to be evaluated. Based on observational studies, desirable baseline 25(OH)D levels are below 40 nmol/L, and, after supplementation, above 75-100 nmol/L.
Major vitamin D RCTs underway
There are five major vitamin D RCTs with adults underway. The relevant information regarding these trials is presented in Table 3. All will have at least 5000 participants, use at least 1600 IU/d in the vitamin D arm, and last for at least five years. It is not clear how many of them are measuring 25(OH)D levels of the participants at baseline. However, there are no restrictions on baseline 25(OH)D levels for participants, but there are limitations on the amount of vitamin D supplements that can be taken. In the U.S., the limitations are from the IOM Report, i.e., 600 IU/d for those under the age of 71 years, 800 IU/d for those older than 71 years. The mean baseline 25(OH)D levels for the various studies were estimated from reports in the literature for elderly people in the countries where the studies are being conducted.
The data are plotted in Figure 1. The linear regression fit to the data lies closer to the fit to the vitamin D RCTs that failed than to the ones that succeeded. However, two of the studies apparently have a significant number of participants who are expected to have baseline 25(OH)D levels below 50 nmol/L, one in Finland (FIND) and one in the U.S. for the 5000 African Americans being enrolled (VITAL). While there is uncertainty whether the trials will find beneficial effects for vitamin D supplementation for those with 25(OH)D levels above 50 nmol/L, when pooled together, the likelihood of finding significant beneficial non-skeletal effects will certainly increase.
The estimates for detecting the effect of vitamin D in reducing the risk of disease was estimated for the VITAL study [Manson, 2012]. In their Table 1, the power for the effects of vitamin D were estimated for cancer for various observed relative risks (RRs). While no estimates were provided for the expected RR, it can be estimated from existing observational study results along with estimated baseline 25(OH)D levels of the participants. From NHANES data for 2001-4, the 25(OH)D levels for whites over the age of 60 years was 63 nmol/L, while for blacks, it was 41 nmol/L [Ginde, 2009]. Assuming 25% blacks and 75% whites, the average baseline 25(OH)D level is expected to be 58 nmol/L. For 2000 IU/d vitamin D, the 25(OH)D levels for whites should increase to 103 nmol/L while for blacks, to 88 nmol/L [Garland, 2011], for a combined average of 99 nmol/L. The 25(OH)D-cancer incidence and mortality rate relations can be estimated several ways. One is to use the 25(OH)D level-incidence relations for breast and colorectal cancer [Grant, 2010]. That approach yields an odds ratio of 0.75. However, since 15% of non-skin cancer cases are due to lung and related cancers in the U.S. [Siegel, 2014], and since some of other cancers may not be vitamin D sensitive, the odds ratio changes to 0.80-0.85. A second way is to use the RR value for an increase in 25(OH)D level of 25 nmol/L found in the Health Professionals Follow-up Study was 0.84 (0.72-0.98) [Giovannucci, 2006]. That would lead to an estimate of 0.70 for a 41 nmol/L change, assuming the 25(OH)D level-colorectal cancer incidence relation and a low 25(OH)D level of 55 nmol/L. The cancer mortality rate RR was 0.69 (0.55-0.86) in that study. Thus, the range of RR for cancer incidence rates is from 0.70 to 0.85 plus the uncertainty of these values, and the range of RR for cancer mortality rates ranges from about 0.50 to 0.70 plus the uncertainty of these values. From Table 1 in Mason [2012], the power for detecting the effect of vitamin D on cancer incidence ranges from 86% to 99.9%, while that for cancer mortality ranges from 78% to 96%.
For CVD, the 25(OH)D level-CVD incidence relation is available as a meta-analysis of observational studies [Wang, 2012]. For baseline and final 25(OH)D levels of 58 and 99 nmol/L, the expected RR is 0.90. From Table 2 in [Manson, 2012], this gives a power effect of 35% for major CVD and 53% for total CVD. Most of the effect of increasing 25(OH)D levels should come from the 5000 African Americans. Based on their expected baseline and final 25(OH)D levels, the RR for CVD for African Americans should be about 0.7 . Thus, it appears more likely that the VITAL study will find beneficial effects for cancer than for CVD.
Comment by Vitamin D Life – Because VITAL is not providing enough Vitamin D to achieve CVD benefits
References for all sections
Grant WB. Using findings from observational studies to guide vitamin D randomized controlled trials. J Intern Med. 2014 Apr 15. doi: 10.1111/joim.12260. [Epub ahead of print] (PDF is behind paywall, so it is not on Vitamin D Life)
Heaney RP. Guidelines for optimizing design and analysis of clinical studies of nutrient effects. Nutr Rev. 2014 Jan;72(1):48-54.in Vitamin D Life
Lappe JM, Heaney RP. Why randomized controlled trials of calcium and vitamin D sometimes fail. Dermatoendocrin. 2012;4(2):95-100. in Vitamin D Life
Armstrong B, Doll R. Environmental factors and cancer incidence and mortality in different countries, with special reference to dietary practices. Int J Cancer. 1975 Apr 15;15(4):617-31.
Cho E, Chen WY, Hunter DJ, Stampfer MJ, Colditz GA, Hankinson SE, Willett WC. Red meat intake and risk of breast cancer among premenopausal women. Arch Intern Med. 2006 Nov 13;166(20):2253-9.
Grant WB. A multicountry ecological study of cancer incidence rates in 2008 with respect to various risk-modifying factors, Nutrients. 2014;6(1):163-189.
Rebel H, Dingemanse-van der Spek C, Salvatori D, van Leeuwen JP, Robanus-Maandag EC, de Gruijl FR. UV exposure inhibits intestinal tumour growth and progression to malignancy in intestine-specific Apc mutant mice kept on low vitamin D diet. Int J Cancer. 2014 May 29. doi: 10.1002/ijc.29002. [Epub ahead of print]
Garland CF, French CB, Baggerly LL, Heaney RP. Vitamin D supplement doses and serum 25-hydroxyvitamin D in the range associated with cancer prevention. Anticancer Res 2011:31: 617-22. PDF in Vitamin D Life
Ginde AA, Liu MC, Camargo CA Jr. Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004. Arch Intern Med. 2009 Mar 23;169(6):626-32.
Giovannucci E, et al. Prospective study of predictors of vitamin D status and cancer incidence and mortality in men. JNCI 2006; 98:451-9.
Grant WB. Relation between prediagnostic serum 25-hydroxyvitamin D level and incidence of breast, colorectal, and other cancers. J Photochem Photobiol B. 2010;101:130-136.
Manson JE, et al. The VITamin D and OmegA-3 TriaL (VITAL): rationale and design of a large randomized controlled trial of vitamin D and marine omega-3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease. Contemp Clin Trials. 2012 Jan;33(1):159-71.
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014 Jan-Feb;64(1):9-29.
Wang L, et al. Circulating 25-hydroxy-vitamin D and risk of cardiovascular disease: A meta-analysis of prospective studies. Circ Cardiovasc Qual Outcomes. 2012 Nov 1;5(6):819-29. In Vitamin D Life
PDF of the large poster is attached at the bottom of this page
