Intestinal absorption of vitamin D - a systematic review
Nutrition Reviews VR Vol. 0(0):1–17, doi: 10.1093/nutrit/nux034
Mariana Costa Silva and Tania Weber Furlanetto
📄 Download the PDF from Vitamin D Life
Context: Vitamin D is frequently prescribed as a supplement, yet its absorption remains poorly understood.
Objective: This systematic review was performed to evaluate data on mechanisms involved in the intestinal absorption of vitamin D.
Data Sources: PubMed, Embase, and Cochrane Library databases were searched.
Study Selection: The following studies were included: experimental laboratory studies of vitamin D absorption through the enterocyte brush-border membrane; absorption tests that used radiolabeled vitamin D; and clinical trials in adults that investigated a single dose of cholecalciferol or ergocalciferol and reported at least 2 measurements of serum cholecalciferol, ergocalciferol, or 25-hydroxyvitamin D.
Data Extraction: From 2069 articles identified, 46 met the inclusion criteria.
Results: Different methods were employed to evaluate vitamin D absorption. Recent research suggests that vitamin D absorption is not an exclusive simple diffusion process. Vitamin D was better absorbed when it was consumed with fat- containing meals, but absorption also occurred without fat or oily vehicles. Factors that modified cholesterol absorption also altered vitamin D absorption.
Conclusion: Vitamin D is probably absorbed through passive diffusion and a mechanism involving membrane carriers, especially cholesterol transporters, although data remain scarce. Some data suggest that fat, when consumed concomitantly with vitamin D, improves vitamin D absorption.
INTRODUCTION
Vitamin D deficiency is a global concern, particularly because of the importance of vitamin D in bone health and other systemic functions.1-4 Vitamin D is a steroid prohormone that can be supplied by skin synthesis in humans when skin is exposed to ultraviolet B radiation.5 Many people, however, require dietary vitamin D supplements, mainly because of low sun exposure. Recently, researchers have shown an increased interest in the physiology and metabolism of vitamin D, especially with regard to the absorption of orally ingested vitamin D.
Until recently, it was accepted that vitamin D was absorbed by means of a simple passive diffusion process. Now, however, it is thought that absorption may occur through complex mechanisms of vitamin D incorporation.
Passive diffusion has been observed with pharmacological doses of vitamin D,6 and clinical trials have demonstrated that vitamin D was absorbed even when ingested with nonfat meals or nonoily vehicles7,8 or during fasting.9
This systematic review includes studies that evaluated the intestinal absorption of vitamin D. An electronic search of the literature was conducted up to January 2016 using Ovid MEDLINE, Embase, and the Cochrane Library by combining the MeSH terms “vitamin D” and “absorption.” Knowing how vitamin D is absorbed, as well as the factors that might interfere
Affiliation: M.C. Silva and T.W. Furlanetto are with the School of Medicine, Postgraduate Program in Medicine: Medical Sciences, Federal University of Rio Grande do Sul, Porto Alegre, Rio Grande do Sul, Brazil. T.W. Furlanetto is with the Internal Medicine Division, Hospital de Clinicas de Porto Alegre, Porto Alegre, Brazil.
Correspondence: T.W. Furlanetto, Internal Medicine Division, Hospital de Clinicas de Porto Alegre, Rua Ramiro Barcelos, 2350/700—90035903, Porto Alegre, RS, Brazil. Email: [email protected].
Table 1 PICOS criteria for the inclusion and exclusion of studies
METHODS
This review followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines.10 The Population, Intervention, Comparison, Outcomes, and Study design (PICOS) criteria were used to formulate and narrow the focus of the following research question: What mechanisms are involved in the intestinal absorption of vitamin D (Table 1)?
Identification of studies
Original research studies were identified from the databases PubMed, Embase, and the Cochrane Library, using the combination of medical subject headings (MeSH) “vitamin D” and “absorption.” Search details were as follows: (“vitamin D/administration and dosage”[MeSH] OR “vitamin D/pharmacokinetics”[MeSH] OR “vitamin D/ physiology”[MeSH]) AND (“absorption”[MeSH terms] OR “absorption”[all fields]).
Criteria for inclusion and exclusion of studies
All original studies in English, Portuguese, and Spanish, published up to January 2016, were considered for this review. The following types of studies were included: experimental laboratory studies of vitamin D absorption through the enterocyte brush-border membrane; absorption tests that used radiolabeled vitamin D; and clinical trials of a single dose of cholecalciferol or ergocalciferol that reported at least 2 measurements of serum cholecalciferol, ergocalciferol, or 25-hydroxyvitamin D [25(OH)D]. Studies were excluded if they were performed in a pediatric sample or were published within a systematic review, book chapter, conference proceedings, correspondence, or authors’ comments.
Data extraction
Both authors screened the titles and abstracts identified from the electronic search. In the event the reviewers disagreed about an abstract, the abstract was reevaluated and disagreement was resolved by discussion and consensus. Full texts were obtained and were again evaluated for eligibility by the authors. Additional papers were identified by cross-referencing the texts. Study quality was not rated because of differences in the study design. No meta-analyses were performed.
RESULTS
Studies of vitamin D absorption
From 2069 titles and abstracts, 109 articles were selected for full-text review. Of these, 79 were excluded because of study design. Thus, 30 studies were included, as well as 16 others obtained by cross-referencing articles (Figure 1). All 46 studies fulfilled 1 of the 3 inclusion criteria and, subsequently, were classified into the following groups: 16 laboratory experiments that investigated vitamin D absorption through the enterocyte apical membrane (Table 26’11-25); 9 absorption tests that used radiolabeled vitamin D (Table 326-34); and 21 clinical trials of a single dose of vitamin D, 8 of which were performed in adults with compromised health (Table 435-42) and 13 of which were performed in healthy adults (Table 57-9,43-52).
DISCUSSION
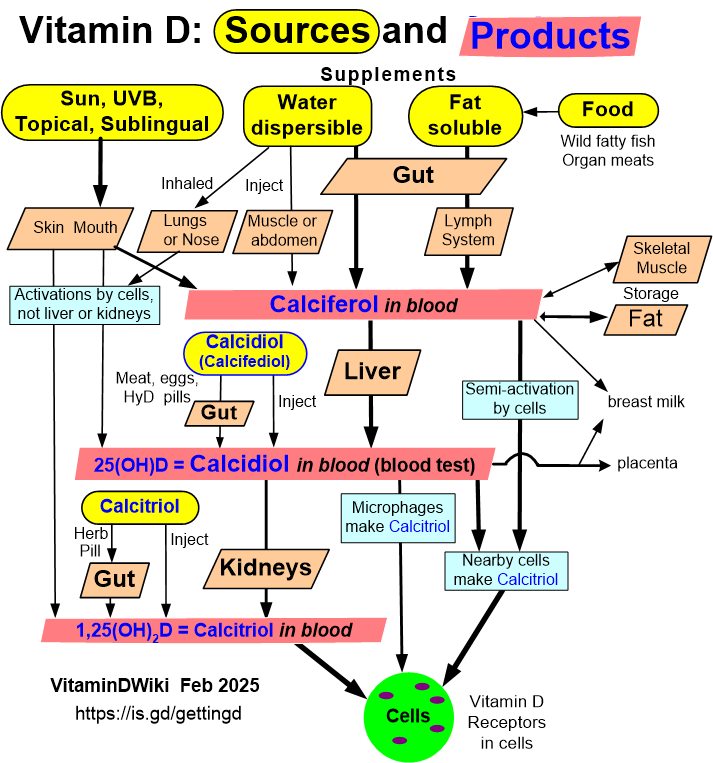
Ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3) are the preparations commonly prescribed to prevent and treat vitamin D deficiency.53 The former is a plant-derived form of vitamin D and the latter is the animal-derived form of vitamin D, which can be synthesized by irradiation of 7-dehydrocholesterol in the skin by ultraviolet B (UVB) light. Both forms are similar in structure, and both need to be hydroxylated to 25(OH)D within the liver and to 1,25dihydroxyvitamin D [1,25(OH)2D], the active form, in the kidneys.54
Different forms of vitamin D and different methods were used to evaluate vitamin D absorption. Altogether, the selected studies provided insight into the mechanisms involved in vitamin D intestinal absorption.
Figure 1 Flow diagram of the literature search process.
Basic science research
Table 2 provides an overview of the experimental in vivo and in vitro studies of vitamin D uptake through the apical membrane of the enterocytes.
Current knowledge of vitamin D uptake through the brush-border (apical) membrane of the enterocytes was obtained from experimental studies in the mid- 1970s, when Hollander et al.23,24 demonstrated a linear relationship between the rate of vitamin D absorption and the intraluminal concentration of vitamin D in 2 studies using everted gut sacs and live rats. Moreover, those authors demonstrated that the absorption rate was raised by an increase in either the flow rate of the perfusate or the hydrogen ion concentration, which decreased the resistance of the cell membrane to the diffusion of micelles. These results indicated a lack of saturation kinetics and supported the idea of vitamin D absorption by passive diffusion.
For many years, the mechanistic process of vitamin D intestinal uptake was no longer the emphasis of investigations, and laboratory experiments focused only on factors that could interfere with vitamin D uptake, such as uremia,19 gastrectomy,18 aging,17,21,22 and vitamin D status.16 For example, the effect of aging on intestinal absorption of vitamin D was evaluated in 3 experimental studies, 2 of which indicated that age had no significant impact on vitamin D absorption in rats.17,21
The influence of vitamin D status on the intestinal absorption and body retention of vitamin D was evaluated by Lorentzon and Danielson.16 Radiolabeled cholecalciferol ([3H]D3) was administered intragastrically to rats fed previously with different amounts of vitamin D. Animals with vitamin D deficiency accumulated high levels of serum radioactivity, which were to a great extent confined to polar fractions of 25(OH)D and 1,25(OH)2D, with less radioactivity found in the 3- day fecal collection from these animals. These results suggested that intestinal absorption of vitamin D might be greater in states of vitamin D deficiency.
In a wider perspective, Bikhazi and Hasbini15 investigated the brush-border mechanistic passage of vitamin D and its metabolite 1,25(OH)2D. Radiolabeled cholecalciferol ([14C]D3) and 1,25(OH)2D ([3H]1,25D3) were measured in intestinal perfusates and portal blood samples of rats injected with cycloheximide, an inhibitor of protein and chylomicron synthesis. The amount of [14C]D3 lost from the perfusate was similar in the experimental and control groups. The treated rats, however, showed a drastic increase in [14C]D3 retention in the intestine and a reduction in [14C]D3 portal plasma. The authors concluded that cholecalciferol might be transferred through the cytosol by carrier-binding proteins. Moreover, they observed that apical membrane absorption was different for cholecalciferol and 1,25(OH)2D, since [3H]1,25D3 uptake from the perfusates was significantly reduced in cycloheximide-treated rats.15
Sitrin and Bengoa27 demonstrated that 25(OH)D, another polar metabolite of vitamin D, had an improved absorption pattern compared with cholecalciferol, both in patients with chronic cholestatic liver disease and in healthy persons. Although the mechanistic processes are not clear, other experiments in humans and in rats suggested that intestinal absorption of 25(OH)D was less dependent on chylomicron production and release than was intestinal absorption of cholecalciferol.20,29
More than 30 years after the first experiments about intestinal uptake of vitamin D, researchers observed that cholesterol and vitamin D had similar absorption mechanisms .6,11-13 These studies demonstrated that cholesterol and factors that are known to interfere with cholesterol uptake, such as phytosterols and long-chain fatty acids, also reduced the absorption of vitamin D in experimental models. 12,13,25
Great advances in knowledge about cholesterol absorption have been made in recent decades. It is now well recognized that cholesterol absorption involves protein membrane transporters.55 The most important cholesterol membrane carrier is the Niemann-Pick C1- like 1 carrier (NPC1L1),55 followed by scavenger receptor class B type I (SR-BI),56 cluster determinant 36 (CD36), and ATP-binding cassette transporter A1.57
Reboul et al.6 evaluated vitamin D uptake in human Caco-2 cells, which are models of human intestinal epithelium often employed in the assessment of intestinal transport of lipids, and in human embryonic kidney (HEK) 293T cells, which are validated models of SR-BI, CD36, and NPC1L1 overexpression. Vitamin D uptake was higher in transfected HEK 293T cells and decreased after administration of carrier-specific inhibitors. Both ezetimibe, a pharmacological NPC1L1 inhibitor, and an SR-BI inhibitor similarly reduced the uptake of vitamin D in Caco-2 cells. In live mice treated with eze- timibe, vitamin D absorption decreased nonsignificantly in a study conducted by van Heek et al.14
Gonsalves et al.12 found that long-chain fatty acids, which modulate cholesterol absorption, interfered with vitamin D absorption . They postulated a possible modification in the micellar electrical charge or a modulation of cholecalciferol outflow through the basolateral membrane of enterocytes as a potential mechanism for the reduction in vitamin D absorption. Another possible explanation offered was the competition between free fatty acids and cholecalciferol for the same transporter, especially CD36 or SR-BI, since these 2 proteins are known to be involved in fatty acid uptake.
Phytosterols are commonly employed to reduce dietary cholesterol absorption, and the same research group evaluated, both in vitro and ex vivo, the effects of different sterols on micellar incorporation of cholecalciferol, apical uptake of cholecalciferol, and basolateral efflux.13 In mice, cholecalciferol bioavailability was 15-fold lower in the presence of b-sitosterol (P < 0.05) . The significantly impaired cholecalciferol incorporation into mixed micelles (from —16% to —36%. depending on the sterol micellar composition) and the significantly lowered cholecalciferol apical uptake (from —13% to —39%) were cited by the authors as possible causes for the decreased vitamin D bioavailability. They also observed vitamin D and phytosterol competition for a common membrane transporter, supposedly NPC1L1.
Clinical research: radiolabeled absorption tests
Administering radiolabeled forms of vitamin D and then monitoring vitamin D levels in blood, tissues, urine, and feces is the most direct way to evaluate vitamin D absorption. Studies of intestinal absorption of radiolabeled forms of vitamin D in humans are shown in Table 3 and will be described in this section.
Thompson et al.34 were the first group to describe a protocol for the assessment of vitamin D absorption in humans. The protocol consisted of administering a single oral dose of [3H]D3 to healthy individuals or to patients with different gastrointestinal diseases and then monitoring total plasma radioactivity over a 4-day period. They found higher plasma radioactivity levels 6 to 12 hours after [3H]D3 administration, with lower plasma radioactivity concentrations in patients with steatorrhea or celiac disease.
Similarly, different malabsorptive conditions such as severe cholestasis,27,28,32 short bowel disease,26,30 and inflammatory bowel disease26 were evaluated in 6 subsequent studies that included control groups. These diseases did not seem to interfere with the time to reach the peak plasma level of vitamin D, with the highest concentrations observed about 6 to 24 hours after oral administration.26-32 However, they did seem to modify absorption, with lower plasma levels observed in patients with malabsorptive conditions than in control groups. The wide range of time in which the vitamin D plasma peaks were detected was possibly related to different study protocols, different vitamin D plasma measurements, and other noncontrolled factors such as different degrees of malabsorption or different gastrointestinal transit times in patients.
Parallel to patients with malabsorptive disease, hospitalized elderly patients also had lower plasma radioactivity concentrations compared with healthy adults.31 On the other hand, plasma radioactivity and the shape of the radioactive peak and decline were similar in patients taking anticonvulsants and in healthy individuals.33
In addition, the intestinal absorption of labeled cholecalciferol was compared with that of labeled 25(OH)D ([3H]25(OH)D3) in 3 different studies involving patients with multiple gastrointestinal diseases and control groups.26,27,30 Administration of [3H]25(OH)D3 resulted in higher serum radioactivity levels, which also peaked faster than after the administration of labeled cholecalciferol. Therefore, apparently 25(OH)D is better absorbed than its less polar precursor (cholecalciferol or ergocalciferol) in individuals with inflammatory bowel disease or cholestasis. Additionally, Compston et al.29 observed, in healthy men, that 25(OH)D absorption might be independent of bile acids , with some absorption occurring directly into the portal vein.
In another study, Danielsson et al.28 investigated whether hepatic hydroxylation is altered in patients with primary biliary cirrhosis . They assessed levels of radiolabeled 25(OH)D ([3H]25(OH)D3) in serum after [3H]D3 administration in women with primary biliary cirrhosis and in a control group. The response was similar in both groups, with a gradual increase in [3H]25(OH)D3 levels observed as [3H]D3 levels declined, showing that hepatic hydroxylation of vitamin D was not impaired in that population.
Clinical trials
Clinical trials using a single nonlabeled dose of ergocalciferol or cholecalciferol showed results to those of studies using radioactive forms of ergocalciferol. As ergocalciferol is rarely found in the human diet and is not synthesized by human skin, it is more suitable than cholecalciferol for use in vitamin D absorption tests. The aim of these studies was, in general, to assess the impact of diseases (Table 4) or the influence of dietary compounds (Table 5) on vitamin D absorption.
Impact of disease on vitamin D absorption.
Lo et al.42 were the first group to evaluate the plasma levels after a high dose of nonlabeled ergocalciferol, calling it a challenge test. A capsule containing 50 000IU of ergocalciferol was offered to 7 patients with clinical fat malabsorptive conditions (cystic fibrosis, Crohn disease, villous atrophy, scleroderma, and ulcerative colitis) and to 7 healthy volunteers. In the healthy group and in 2 patients with malabsorption, plasma ergocalciferol levels increased within 4 hours and peak concentrations were reached by 12 hours, gradually declining to baseline levels within 3 days. In marked contrast, there was no increase in ergocalciferol levels in the other 5 patients with malabsorption.
Similarly, Lark et al.39 and Farraye et al.35 conducted ergocalciferol challenge tests in patients with cystic fibrosis and Crohn disease , respectively. Like Lo et al.,42 both groups also found lower ergocalciferol levels when the unhealthy groups were compared with their respective control groups. It is important to note that there was wide variability in the responses of individual persons.
Besides analyzing ergocalciferol concentrations, Lark et al.39 examined the 25(OH)D response to a single oral dose of 100 000 IU of ergocalciferol in cystic fibrosis and control groups over 36 hours. In both groups, maximal levels of ergocalciferol were detected in plasma around 24 hours after ergocalciferol administration. As serum ergocalciferol levels gradually declined, serum 25(OH)D levels increased in the control group. In the cystic fibrosis group, 25(OH)D concentrations did not increase significantly at any time .
Roux-en-Y bariatric surgery also altered cholecalciferol absorption in a study by Aarts et al.36 The difference between the baseline level and the highest postabsorptive cholecalciferol level after a single dose of 50 000 IU of cholecalciferol decreased from 92.0 ± 6.5 to 63.5 ± 10.3 nmol/L after bariatric surgery (P < 0.02), although results varied markedly between patients.
On the other hand, young women with anorexia nervosa had a similar response to a single dose of oral ergocalciferol compared with healthy-weight controls, despite their severe malnutrition, in a study by DiVasta et al.37 Moreover, obesity did not seem to interfere with vitamin D absorption. Peak ergocalciferol concentrations, the difference between peak and basal concentrations, and mean serum 25(OH)D levels were similar in obese and normal body mass index groups in a study by Wortsman et al.40 However, body mass index was inversely correlated with peak serum ergocalciferol concentrations after ergocalciferol intake (r = —0.56; P = 0.007). The authors concluded that obesity- associated vitamin D insufficiency is likely due to the decreased bioavailability of vitamin D deposited in body fat compartments.
Aging also did not seem to interfere with vitamin D absorption . Clemens et al.41 found similar plasma ergocalciferol peak levels after a single oral dose of 50 000 IU of ergocalciferol in young volunteers and in institutionalized elderly with normal kidney function. Additionally, von Restorff et al.38 analyzed serum 25(OH)D levels after a single oral dose of 300 000 IU of cholecalciferol in elderly persons with vitamin D deficiency. This intervention increased serum 25(OH)D concentrations in most patients to at least 50 nmol/L, and 48% of patients reached the desirable level of at least 75 nmol/L at 3 months. Despite a decline at 6 months, mean 25(OH)D levels were still more than 4 times higher when compared with baseline levels.
Overall, these results highlight the need for caution when interpreting data about vitamin D absorption in health disorders, since several other factors not directly related to the intestinal uptake of vitamin D might interfere with the plasma vitamin D response. For instance, lower serum 25(OH)D levels are commonly found in inflammatory conditions, even when the gastrointestinal tract is not affected.58
Possible reasons for lower serum 25(OH)D levels include
an altered concentration or activity of the 25-hydroxylase enzyme,
a decrease in the concentration of vitamin D-binding protein, or
higher rates of metabolic clearance of 25(OH)D.
Vitamin D absorption in healthy individuals.
Although measurement of serum 25(OH)D could be less sensitive to variations in vitamin D absorption than measurement of serum calciferol, especially during sickness, it has been proven to be a good tool for evaluating both vitamin D status and the effect of vitamin D supplementation in healthy people.47,52
Ellis and Cooke52 were the first group to evaluate the serum 25(OH)D levels in healthy individuals before and at intervals after a single oral dose of 40 000 IU of cholecalciferol. They compared the 25(OH)D response in 2 groups—7 Indian immigrants and 8 Europeans— and found an immediate increase in serum 25(OH)D concentrations after the oral dose in both groups. Over the first 5 days, the mean increase was greater in the Indians than in the Europeans, possibly due to lower 25(OH)D baseline levels in the Indian group.
Subsequently, Armas et al.49 evaluated the pharmacological effects of cholecalciferol and ergocalciferol by administrating 12 weekly doses of 50 000 IU of the respective calciferols to 20 healthy male volunteers. Both calciferols produced similar rises in the serum concentration of the administered vitamin, indicating equivalent absorption. Similar initial rises in serum 25(OH)D were observed over the first 3 days, but 25(OH)D continued to rise in the cholecalciferol-treated men, peaking after 14 days, while serum 25(OH)D fell rapidly in the ergocalciferol-treated men and was not different from baseline after 14 days. The authors suggested that the potency of ergocalciferol is less than one-third that of cholecalciferol.
In a different approach, Whyte et al.51 compared the effect of single doses of vitamin D2 or D3 administered
orally,
subcutaneously,
intramuscularly, or
intravenously
to healthy volunteers on 25(OH)D levels. Similar increases in serum 25(OH)D levels were noted after both intravenous D2 and intravenous D3. Subcutaneous and intramuscular injection of vitamin D in oil resulted in delayed serum 25(OH)D increases compared with oral and intravenous administration.
Moreover, Ilahi et al.47 evaluated the pharmacological effects of a single large dose of cholecalciferol (100 000 IU) in healthy people. Peak plasma concentrations of cholecalciferol were reached 8 to 24 hours after administration, while the highest plasma 25(OH)D concentrations were observed 7 days after cholecalciferol administration. It is interesting to note that the peak plasma concentrations of 25(OH)D were reached faster in this study of a single 100 000 IU cholecalciferol dose than in the earlier study of a single 50 000 IU cholecalciferol dose.47
Recent studies aimed to evaluate the influence of fat-containing meals on the absorption of cholecalciferol.7,8,44,45 Raimundo et al.8,45 conducted 2 randomized controlled trials about the influence of dietary fat on the absorption of a single 50 000 IU oral dose of cholecalciferol. In the more recent study, young medical doctors were divided into 3 groups according to the fat content of meals (0 g, 15 g, or 30 g of fat) given with the cholecalciferol dose or placebo.8 Mean serum 25(OH)D concentrations were higher in those who received lunch containing at least 15 g of fat, but the group that received the fat-free meal also showed increased 25(OH)D levels when compared with the placebo group.
Following laboratory experiments in which polyunsaturated fatty acids were demonstrated to decrease vitamin D absorption, Dawson-Hughes et al.7 tested whether the ratio of monounsaturated fatty acids to polyunsaturated fatty acids in food modified vitamin D absorption in men and postmenopausal women, all older than 50 years. They found that the ratio had no significant influence on vitamin D absorption in this population.
Holmberg et al.50 showed that cholecalciferol was absorbed more efficiently in the fasting state when incorporated in peanut oil containing long-chain fatty acids than when incorporated in a medium-chain triglyceride, although there was no difference between the 2 formulations when cholecalciferol was administered with food.
Johnson et al.48 investigated whether the bioavailability of ergocalciferol in cheese was similar to that of ergocalciferol dissolved in water and compared the absorption in younger vs older adults. They concluded that ergocalciferol was absorbed more efficiently from cheese than from water and that age had no impact on absorption. Conversely, Wagner et al.46 demonstrated, by measuring serum 25(OH)D levels, that the bioavailability of cholecalciferol in fortified cheese and in a liquid supplement, taken either with or without food, was similar.
Denker et al.9 evaluated the absorption of cholecalciferol doses as low as 5600 IU and 2800 IU. Doses were administered following an overnight fast, and participants continued to fast for 2 hours. The aim of the study was to evaluate if the alendronate component of an alendronate/cholecalciferol combination tablet was bioequivalent to a 70-mg alendronate tablet and if the pharmacokinetic parameters of cholecalciferol were similar with and without alendronate. The bioavailability of alendronate and cholecalciferol was similar in the combination tablet and when administered alone. Notably, cholecalciferol absorption was observed even with nonfat meals and nonoily vehicles.
Clinical trials addressing factors that might interfere with vitamin D absorption are scarce. Silva et al.43 conducted a randomized, double-blind, placebo-controlled trial intended to determine if the NPC1L1 cholesterol transporter participates in vitamin D absorption. They examined the effect of ezetimibe on serum 25(OH)D levels 14 days after a single oral dose of 50 000IU of cholecalciferol in healthy young volunteers. The mean change in serum 25(OH)D 14 days after cholecalciferol was not affected by ezetimibe. As already noted, similar results were demonstrated in live mice, supporting the notion that NPC1L1 probably is not an important vitamin D transporter.6
Currently, ezetimibe is the only pharmacological inhibitor of cholesterol transporters available for clinical use. This is probably why no clinical studies evaluating the effect of inhibition of other cholesterol transporters, such as SR-BI and CD36, on vitamin D absorption have been performed yet.
CONCLUSION
This systematic review was designed to consolidate and interpret data on the mechanisms of vitamin D absorption, with emphasis on vitamin D uptake through the apical membrane of enterocytes. The reviewed studies revealed some distinctive aspects of vitamin D bioavailability that should be considered when treating or preventing vitamin D deficiency. Ergocalciferol and cholecalciferol, the vitamin D preparations commonly prescribed, are both rapidly absorbed after oral intake, with maximum plasma levels detected around 24 hours after administration. Levels of 25(OH)D increase gradually, peaking at approximately 7 to 14 days, depending on the dose of vitamin D administered. Cholecalciferol seems to be more potent than ergocalciferol, resulting in more sustainable levels of serum 25(OH)D. Absorption is improved when vitamin D is given with fat-containing food and is impaired by intestinal fat malabsorption. Neither aging nor obesity, however, alters vitamin D absorption.
other studies disagree: aging decreases both oral Vitamin D and vitamin D from the sun
Different forms of vitamin D and various methods were employed to evaluate the absorption of vitamin D. Clinical trials using a single nonlabeled dose of ergocalciferol or cholecalciferol showed results similar to those of studies using radiolabeled vitamin D. Although measurement of serum 25(OH)D is less sensitive than measurement of serum cholecalciferol for detecting minor variations in vitamin D absorption, especially during illness, it was demonstrated to be a good tool for evaluating the effect of vitamin D supplementation in healthy people. Moreover, recent in vivo experiments and in vitro studies demonstrated that vitamin D absorption is not exclusively a simple diffusion process, as previously assumed, but rather a mechanism that involves membrane carriers. Cholesterol transporters may also be responsible for vitamin D uptake, since factors interfering with cholesterol absorption also interfered with vitamin D absorption in laboratory and clinical studies. However, although NPC1L1 is the major cholesterol transporter, it did not seem to play a fundamental role in vitamin D absorption in studies using live rodents or in a clinical trial in which ezetimibe was administered to healthy adults.
This systematic review is limited by the heterogeneity of the included studies, since different methods were used to evaluate vitamin D absorption. Despite recent increased interest in the mechanisms of vitamin D absorption, data on this topic, especially from clinical research, remain scarce. This review provides insight for future research, revealing in particular the need to both identify vitamin D membrane transporters and to translate basic research findings into clinical research.
