Increased mortality associated with low vitamin D genes
Genetically low vitamin D concentrations and increased mortality: mendelian randomisation analysis in three large cohorts
BMJ 2014; 349 doi: http://dx.doi.org/10.1136/bmj.g6330 (Published 18 November 2014)
Shoaib Afzal, registrar12, Peter Brøndum-Jacobsen, registrar12, Stig E Bojesen, professor123, Børge G Nordestgaard, professor123 [email protected]
Objective To test the hypothesis that genetically low 25-hydroxyvitamin D concentrations are associated with increased mortality.
Design Mendelian randomisation analysis.
Note: the editorial in the same issues, further down this page, describes Mendelian randomisation techniques
Setting Copenhagen City Heart Study, Copenhagen General Population Study, and Copenhagen Ischemic Heart Disease Study.
Participants 95 766 white participants of Danish descent from three cohorts, with median follow-up times of 19.1, 5.8, and 7.9 years, genotyped for genetic variants in DHCR7 and CYP2R1 affecting plasma 25-hydroxyvitamin D concentrations; 35 334 also had plasma 25-hydroxyvitamin D measurements. Participants were followed from study entry through 2013, during which time 10 349 died.
Main outcome measures All cause mortality and cause specific mortality, adjusted for common risk factors for all cause mortality based on the World Health Organization’s global health status.
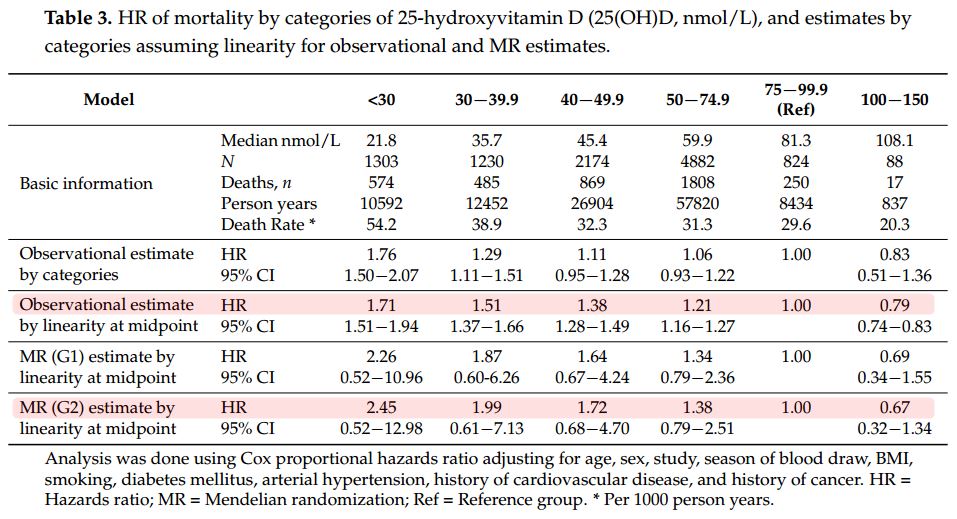
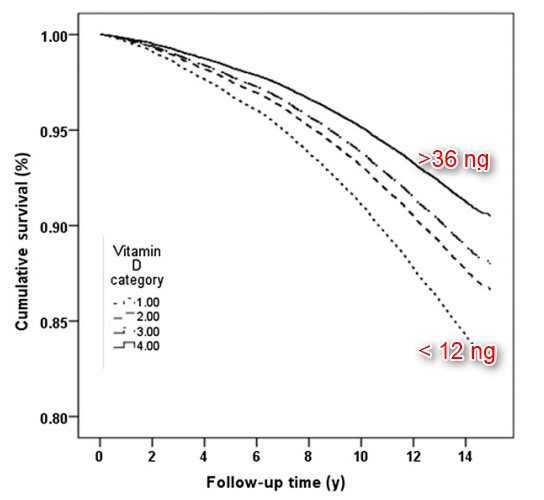
Results The multivariable adjusted hazard ratios for a 20 nmol/L lower plasma 25-hydroxyvitamin D concentration were 1.19 (95% confidence interval 1.14 to 1.25) for all cause mortality, 1.18 (1.09 to 1.28) for cardiovascular mortality, 1.12 (1.03 to 1.22) for cancer mortality, and 1.27 (1.15 to 1.40) for other mortality. Each increase in DHCR7/CYP2R1 allele score was associated with a 1.9 nmol/L lower plasma 25-hydroxyvitamin D concentration and with increased all cause, cancer, and other mortality but not with cardiovascular mortality. The odds ratio for a genetically determined 20 nmol/L lower plasma 25-hydroxyvitamin D concentration was 1.30 (1.05 to 1.61) for all cause mortality, with a corresponding observational multivariable adjusted odds ratio of 1.21 (1.11 to 1.31). Corresponding genetic and observational odds ratios were 0.77 (0.55 to 1.08) and 1.13 (1.03 to 1.24) for cardiovascular mortality, 1.43 (1.02 to 1.99) and 1.10 (1.02 to 1.19) for cancer mortality, and 1.44 (1.01 to 2.04) and 1.17 (1.06 to 1.29) for other mortality. The results were robust in sensitivity analyses.
Conclusions Genetically low 25-hydroxyvitamin D concentrations were associated with increased all cause mortality, cancer mortality, and other mortality but not with increased cardiovascular mortality. These findings are compatible with the notion that genetically low 25-hydroxyvitamin D concentrations may be causally associated with cancer and other mortality but also suggest that the observational association with cardiovascular mortality could be the result of confounding.
Figure 1: Increased Mortality associated with low vitamin D
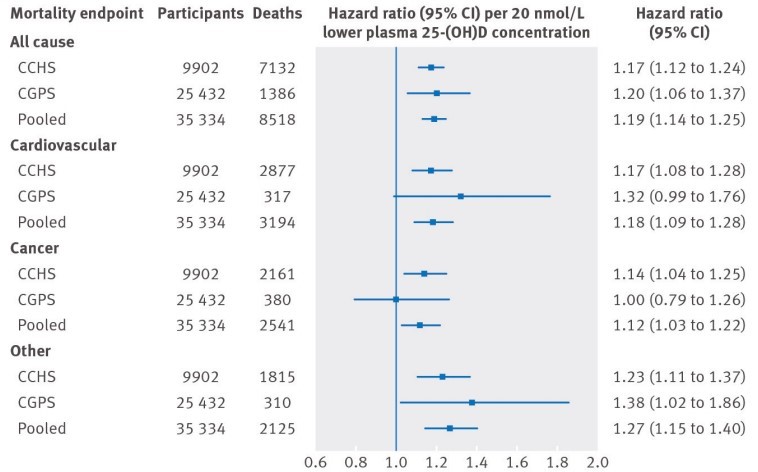
Follow-up time was up to:
32 years in Copenhagen City Heart Study (CCHS)
9.4 years in Copenhagen General Population Study (CGPS).
Figure 3 Increased Mortality associated with just 2 (of over 200) genes
📄 Download the PDF from Vitamin D Life.
BMJ editorial: Vitamin D genes and mortality
BMJ 2014; 349 doi: http://dx.doi.org/10.1136/bmj.g6599 (Published 18 November 2014)
Paul Welsh, British Heart Foundation research fellow, Naveed Sattar, professor of metabolic medicine
Correspondence to: N Sattar [email protected]
Harnessing genetics to re-examine the case for vitamin D
Readers of medical journals would be forgiven for a experiencing a sense of déjà vu—another study investigating of the role of vitamin D in chronic disease, another editorial. They might also be forgiven for thinking that little is left to say about vitamin D that has not already become a cliché. The wealth of research articles written on vitamin D in recent times is not the result of a comedic temporal loop designed to make one feel like Bill Murray relentlessly reliving the same experience in the 1993 cult movie Groundhog Day. Rather it reflects the collective will of the academic community to investigate this topical public health question as rapidly as possible. Afzal and colleagues therefore need make no apology for coming back to the vitamin D question again in the linked paper (doi:10.1136/bmj.g6330), here using a mendelian randomisation approach.1
What is mendelian randomisation , and why might it be better than classical observational epidemiology? We now know that approaches linking circulating 25-hydroxyvitamin D (25-(OH)D) to health outcomes are seriously hampered by confounding and reverse causality.2 The circulating concentration of 25-(OH)D is influenced by factors such as time spent outdoors, diet, adiposity, smoking, and acute phase response. Mendelian randomisation attempts to eliminate such problems by exploiting the random allocation of genetic material at conception.
Take two groups of people within a population, one with a genetic variant or variants leading to lower average circulating 25-(OH)D concentrations for life, the other group without these variants. Any differences in health outcomes between these two groups of people can be attributed to circulating 25-(OH)D; the concentration of this metabolite and its downstream biological effects are the only parameters that should differ systematically between the two groups. All other traits (such as adiposity, smoking, and alcohol intake) should be equally distributed in a large population. This situation then can be viewed as a natural experiment, theoretically analogous to a randomised controlled trial.3
Mendelian randomisation is now being used to help to prioritise drug development targets,3 4 as well as to clarify cause and effect where reliable evidence from randomised controlled trials is difficult to obtain or potentially unethical. Does obesity cause cardiovascular disease? Mendelian randomisation analysis suggests that it does.5 Does modest alcohol intake protect against cardiovascular disease? Mendelian randomisation analysis suggests that it does not.6
Afzal and colleagues’ study comprised 95 766 people from Copenhagen in whom four separate genetic variants were determined, all single nucleotide polymorphisms associated with circulating concentrations of 25-(OH)D. Presence or absence of these variants was then related to risk of death, which occurred in 10 349 people.1 The polymorphisms seem to influence circulating 25-(OH)D through altered enzymatic activity. The authors combined the effects of individual polymorphisms by generating a score to maximise power. Each score increment was associated with a 2% (95% confidence interval 0% to 3%) higher odds of death from any cause and a 3% (0% to 6%) higher odds of death from cancer but no difference in cardiovascular death (2% lower odds; −4% to 1%). The small effect sizes do not diminish the potential importance of these findings in the search for evidence of a causal link between low 25-(OH)D concentrations, disease, and death.
The magnitude of effect of the genetic score on circulating 25-(OH)D is small, and mendelian randomisation studies must include large participant numbers. As a result of the small effect, the authors modelled the anticipated effect of a larger 20 nmol/L reduction in 25-(OH)D and report a 30% (5% to 61%) increase in the odds of death from any cause. These predictions, however, hinge on the primary findings being valid and reliable.
How robust are these findings, and should they alter current thinking about vitamin D and health? The study is well conducted but is subject to potential limitations, as are all mendelian randomisation studies.3 Even if we believe the study to be robust, and despite the narrow confidence intervals around the estimates, the borderline significance of the findings means that we should be careful not to over-interpret. Using the same cohorts, this group recently reported that genetic variants associated with low plasma 25-(OH)D concentrations are associated with type 2 diabetes.7 A more recent mendelian randomisation analysis, with more than five times the number of cases of type 2 diabetes, did not confirm these findings,8 and nor do other data.9 The new study in isolation, albeit focused on mortality and not diabetes, cannot therefore be taken as sufficient evidence to change clinical practice. The epidemiological cliché that “more data are required to confirm these findings” once again applies.
Nevertheless, Afzal and colleagues’ findings provide some cause for optimism about the impending results of large vitamin D trials, more so if they are rapidly confirmed by additional mendelian randomisation studies with greater power. Trials of vitamin D supplementation such as VITAL and FIND will start reporting in 2017,10 11 so we do not have to wait too long to see whether mendelian randomisation studies and large scale trials are in agreement.
Mendelian randomisation is an important emerging research tool, is here to stay, and is beginning to be recognised by guideline committees.12 Of course, in research areas where randomised trials are possible (or indeed ongoing), mendelian randomisation studies should not displace them as the gold standard evidence in clinical guidelines or in the minds of healthcare professionals. In the meantime, there may well be yet more “groundhog days” for vitamin D.
Provenance and peer review: Commissioned; not externally peer reviewed.
References
↵Afzal S, Brøndum-Jacobsen P, Bojesen SE, Nordestgaard BG. Genetically low vitamin D concentrations and increased mortality: mendelian randomisation analysis in three large cohorts. BMJ2014;349:g6330.Abstract/FREE Full Text
↵Welsh P, Sattar N. Vitamin D and chronic disease prevention. BMJ2014;348:g2280.FREE Full Text
- ↵Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet2014;23:R89-98.Abstract/FREE Full Text
↵ Khera AV, Rader DJ. Discovery and validation of new molecular targets in treating dyslipidemia: the role of human genetics. Trends Cardiovasc Med2009;19:195-201.CrossRefMedlineWeb of Science
↵Fall T, Hägg S, Mägi R, Ploner A, Fischer K, Horikoshi M, et al. The role of adiposity in cardiometabolic traits: a mendelian randomization analysis. PLoS Med2013;10:e1001474.CrossRefMedline
↵Holmes M V, Dale CE, Zuccolo L, Silverwood RJ, Guo Y, Ye Z, et al. Association between alcohol and cardiovascular disease: mendelian randomisation analysis based on individual participant data. BMJ2014;349:g4164.Abstract/FREE Full Text
↵Afzal S, Brøndum-Jacobsen P, Bojesen SE, Nordestgaard BG. Vitamin D concentration, obesity, and risk of diabetes: a mendelian randomisation study. Lancet Diabetes Endocrinol2014;2:298-306.CrossRefMedlineWeb of Science
↵Ye Z, Sharp SJ, Burgess S, Scott RA, Imamura F; InterAct Consortium, et al. Association between circulating 25-hydroxyvitamin D and incident type 2 diabetes: a mendelian randomisation study. Lancet Diabetes Endocrinol2014; published online 30 September.
↵Buijsse B, Boeing H, Hirche F, Weikert C, Schulze MB, Gottschald M, ] et al. Plasma 25-hydroxyvitamin D and its genetic determinants in relation to incident type 2 diabetes: a prospective case-cohort study. Eur J Epidemiol2013;28:743-52.CrossRefMedline
↵Manson JE, Bassuk SS, Lee I-M, Cook NR, Albert MA, Gordon D, et al. The VITamin D and OmegA-3 TriaL (VITAL): rationale and design of a large randomized controlled trial of vitamin D and marine omega-3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease. Contemp Clin Trials2012;33:159-71.CrossRefMedlineWeb of Science
↵Finnish Vitamin D Trial (FIND). www.uef.fi/fi/nutritionepidemiologists/find2.
↵Gidding SS, Daniels SR, Kavey RE, for the Expert Panel on Cardiovascular Health and Risk Reduction in Youth. Developing the 2011 Integrated Pediatric Guidelines for Cardiovascular Risk Reduction. Pediatrics2012;129:e1311-9.Abstract/FREE Full Text
Comment by Vitamin D Life
The study found that 1 or 2 genes associated with low vitamin D were not associated with heart problems.
3 other genes associated with low vitamin D have been studied in depth (see below)
291 genes have been found to be affected by just 2,000 IU of vitamin D
2,000 genes apparently have vitamin D receptors.
This study proved that 0.1% of the genes related to low vitamin D are not associated with heart problems.
See also Vitamin D Life
Genetics category listing with associated searches
DHCR7 74 hits as of Nov 2014
Cyp2R1 190 hits Oct 2014,
CPY27A1 107 hits as of Aug 2014
GG and GENE but not Schartz 95 hits as of Nov 2014
GC gene 373 hits as of Oct 2014
CYP24A1 232 hits as of March 2014
Search Vitamin D Life for epigenome OR epigenetics 124 items as of Sept 2014
Mortality category listing with associated searches which includes the following
The TOP articles in Mortality and Vitamin D are listed here:
{category}
Overview Cardiovascular and vitamin D
See also web
- IS LOW VITAMIN D DEADLY? 3 minute video by authors of the study
- Used genetics to eliminate the chicken and egg problem

- Genetically Low Vitamin D Not Linked to CV Death Medscape report on this study
- The headline ignores that the study did find other genetic links between mortality and low vitamin D
- Shame on them for cherry picking the conclusions and ignoring other genes
