VA showed increased vitamin D associated with lower health costs - Lancet
Vitamin D testing – letter to editor
The Lancet, Volume 379, Issue 9827, Page 1700, 5 May 2012 doi:10.1016/S0140-6736(12)60712-0
Alan N Peiris a, Beth A Bailey b, William B Grant c [email protected], Luca Mascitelli d
a Division of Endocrinology, Mountain Home Veterans Administration Medical Center, Medicine Service 111, Mountain Home, TN, USA
b Department of Family Medicine, East Tennessee State University, Johnson City, TN, USA
c Sunlight, Nutrition, and Health Research Center, PO Box 641603, San Francisco, CA 94164, USA
d Comando Brigata Alpina “Julia”, Medical Service, Udine, Italy
Naveed Sattar and colleagues 1 highlight increasing requests for vitamin D measurement and the associated costs. The need to contain health-care costs is universal, especially in western countries where they are increasing at an unsustainable rate. We agree that vitamin D deficiency is prolific worldwide. However, we have major areas of disagreement regarding testing and monitoring of vitamin D.
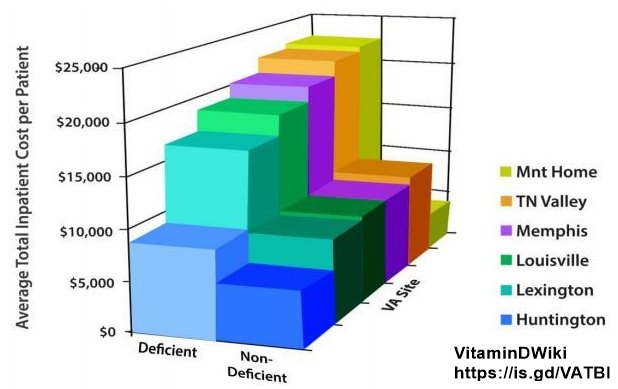
There are many correlates with serum 25-hydroxyvitamin D concentrations, but studies that used common laboratory tests and included latitude and seasonality were unable to predict vitamin D deficiency, suggesting that there is no substitute for 25-hydroxyvitamin D testing.2 We too have noticed a marked increase in testing for vitamin D status in recent years. However, in a study of six Veterans Medical Centers in the southeastern USA, the lowest overall medical costs were in the medical centres that did follow-up vitamin D testing.3 In particular, across all sites, vitamin D deficiency combined with lack of monitoring predicted increased inpatient health-care costs.3
One option to reduce the costs of vitamin D testing would be to supplement the general population with 1000—2000 IU vitamin D3 , as recommended by the Endocrine Society.4 Indeed, such an approach has been postulated to result in a substantial reduction in global health-care costs.5 The greatest benefits accrue to those with serum 25-hydroxyvitamin D concentrations below 50 nmol/L; optimum concentrations should be at least 75—100 nmol/L.4, 5
WBG receives funding from the UV Foundation (McLean, VA, USA), Bio-Tech Pharmacal (Fayetteville, AR, USA), the Vitamin D Council (San Luis Obispo, CA, USA), and the Vitamin D Society (Canada). The other authors declare that they have no conflicts of interest.
References
1 Sattar N, Welsh P, Panarelli M, Forouhi NG. Increasing requests for vitamin D measurement: costly, confusing, and without credibility. Lancet 2012; 379: 95-96. Full Text | PDF(43KB) | CrossRef | PubMed
2 Garland CF, French CB, Baggerly LL, Heaney RP. Vitamin D supplement doses and serum 25-hydroxyvitamin D in the range associated with cancer prevention. Anticancer Res 2011; 31: 617-622. PubMed Contained in Vitamin D Life
3 Bailey BA, Manning T, Peiris AN. Vitamin D testing patterns among six Veterans Medical Centers in the Southeastern United States: links with medical costs. Military Med 2012; 177: 70-76. PubMed Vitamin D Life
4 Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2011; 96: 1911-1930. CrossRef | PubMed Vitamin D Life
5 Grant WB. An estimate of the global reduction in mortality rates through doubling vitamin D levels. Eur J Clin Nutr 2011; 65: 1016-1026. CrossRef | PubMed Vitamin D Life
This letter-to-the-editor and reply by the authors is in one of the PDFs at the bottom of this page
The other PDF is another letter-to-the-editor concerning the same original article
See also Vitamin D Life
VA found less testing for vitamin D resulted in increased health costs – Jan 2012 many of the same authors
Mandatory Vitamin D screening for all patients – vitamin D conference in Middle East – March 2017
Japanese need at least 30 ng of Vitamin D, test costs are now reimbursed – Nov 2016
Medicare now pays for just one vitamin D test , but 20 CT scans for smokers – Feb 2015
All items in category Test for D items
- Many on variation between tests: different days, different testing methods
Vitamin D Life - Cost savings with Vitamin D contains:
{include}