Preterm birth rate reduced by vitamin D – 78 percent if non-white, 39 percent if white
Maternal 25(OH)D concentrations >40 ng/mL associated with 60% lower preterm birth risk among general obstetrical patients at an urban medical center
PLoS ONE 12(7): e0180483. https://doi.org/10.1371/journal.pone.0180483
📄 Download the PDF from Vitamin D Life
Sharon L. McDonnell1, Keith A. Baggerly2, Carole A. Baggerly1, Jennifer L. Aliano1, Christine B. French1 [email protected], Leo L. Baggerly1, Myla D. Ebeling3, Charles S. Rittenberg3, Christopher G. Goodier3, Julio F. Mateus Nino3, Rebecca J. Wineland3, Roger B. Newman3, Bruce W. Hollis3, Carol L. Wagner3
1 GrassrootsHealth, Encinitas, California, USA,
2 Department of Bioinformatics and Computational Biology, The University of Texas MD Anderson Cancer Center, Houston, Texas, USA
3 Medical University of South Carolina Children’s Hospital, Charleston, South Carolina, USA
Background
Given the high rate of preterm birth (PTB) nationwide and data from RCTs demonstrating risk reduction with vitamin D supplementation, the Medical University of South Carolina (MUSC) implemented a new standard of care for pregnant women to receive vitamin D testing and supplementation.
Objectives
To determine if the reported inverse relationship between maternal 25(OH)D and PTB risk could be replicated at MUSC, an urban medical center treating a large, diverse population.
Methods
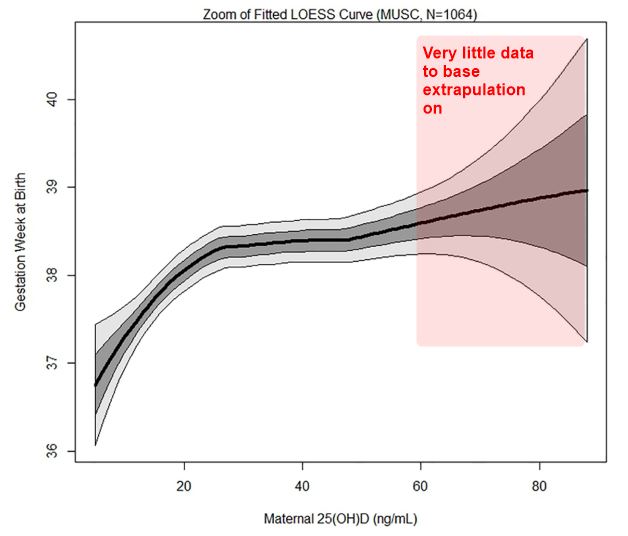
Medical record data were obtained for pregnant patients aged 18-45 years between September 2015 and December 2016. During this time, a protocol that included 25(OH)D testing at first prenatal visit with recommended follow-up testing was initiated. Free vitamin D supplements were offered and the treatment goal was >40 ng/mL. PTB rates (<37 weeks) were calculated, and logistic regression and locally weighted regression (LOESS) were used to explore the association between 25(OH)D and PTB. Subgroup analyses were also conducted.
Results
Among women with a live, singleton birth and at least one 25(OH)D test during pregnancy (N = 1,064), the overall PTB rate was 13%. The LOESS curve showed gestational age rising with increasing 25(OH)D. Women with 25(OH)D >40 ng/mL had a 62% lower risk of PTB compared to those <20 ng/mL (p<0.0001). After adjusting for socioeconomic variables, this lower risk remained (OR = 0.41, p = 0.002). Similar decreases in PTB risk were observed for PTB subtypes (spontaneous: 58%, p = 0.02; indicated: 61%, p = 0.006), by race/ethnicity (white: 65%, p = 0.03; non-white: 68%, p = 0.008), and among women with a prior PTB (80%, p = 0.02). Among women with initial 25(OH)D <40 ng/mL, PTB rates were 60% lower for those with >40 vs. <40 ng/mL on a follow-up test (p = 0.006); 38% for whites (p = 0.33) and 78% for non-whites (p = 0.01).
Conclusions
Maternal 25(OH)D concentrations >40 ng/mL were associated with substantial reduction in PTB risk in a large, diverse population of women.
Supect that the removal of single outlier at 100 ng would greatly reduce the increased risk for vitamin D levels > 60 ng