Cancer patients need more vitamin D, even those who are supplementing – observational study
Cross-sectional observational study - Investigation of vitamin D concentration in Caucasian cancer patients. what is the adequate dose of vitamin D for these patients?
Clin Nutr. 2021 Apr 22;40(6):3852-3858. https://doi.org/10.1016/j.clnu.2021.04.026
Aleksandra Kapała 1, Małgorzata Szlendak 2, Ewelina Grochowska 3
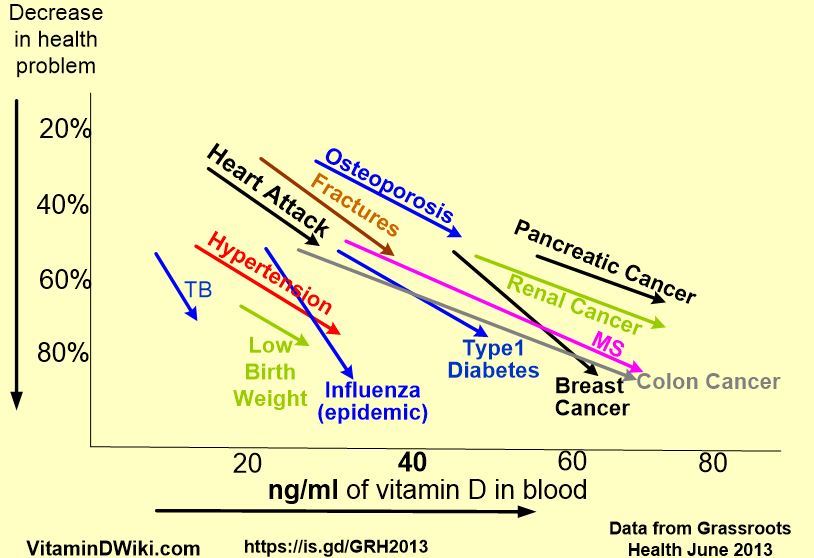 * click on chart for detailsThis study ignored those with dark skins - who often have bigger problems with Cancer* Deaths after Cancer Surgery higher in blacks (probably low vitamin D) – Dec 2020* Blacks are more obese, have lower Vitamin D, and have more Cancer etc. than whites – Feb 2018* Prostate Cancer risk in black men increased 2X having poor Vitamin D Binding Protein – July 2017* Head and Neck Cancer associated with low vitamin D, especially with blacks - April 2012* Overview Dark Skin and Vitamin D has* The health disparity for dark skinned people is almost the same as whites having a low level of vitamin D | | | || --- | --- | --- || | Black
* click on chart for detailsThis study ignored those with dark skins - who often have bigger problems with Cancer* Deaths after Cancer Surgery higher in blacks (probably low vitamin D) – Dec 2020* Blacks are more obese, have lower Vitamin D, and have more Cancer etc. than whites – Feb 2018* Prostate Cancer risk in black men increased 2X having poor Vitamin D Binding Protein – July 2017* Head and Neck Cancer associated with low vitamin D, especially with blacks - April 2012* Overview Dark Skin and Vitamin D has* The health disparity for dark skinned people is almost the same as whites having a low level of vitamin D | | | || --- | --- | --- || | Black vs White | White - low D
vs White - high D || breast cancer | 1.34 | 1.26 || colorectal cancer | 1.43 | 1.44 || cardiovascular disease | 1.29 | 1.27 || all-cause mortality | 1.26 | 1.26 |Many doctors prescribe enough vitamin d for healthy people - post-surgery and chemo patients need much more * Surgeries often deplete Vitamin D - 300,000 IU resulted in little response – Nov 2018Vitamin D even helps after the doctor has given up* Palliative cancer benefit of 4,000 IU of Vitamin D – less opioids, infection, and CRP – Aug 2017Should consider prehabilitation - take Vitamin D BEFORE surgery* Taking Vitamin D just before and after surgery helps (open-heart in this case) – RCT Feb 2021Loading doses of Vitamin D are sometimes used before/after surgeries* 29 studies as of June 2021Cancer category starts with the following{include}--- * Omega-3, Magnesium, Zinc, Quercetin, non-daily Vit D, Curcumin, intense exercise, Ginger, Essential oils, etc** Note: The founder of Vitamin D Life uses 10 of the 12 known VDR activators--- 1. Vitamin D levels drop a lot for a few months following any surgeryVitamin D measured before surgery is not a good indicator of how much vitamin d is needed 1. Vitamin D levels should be > 40 ng or higher at all times* Is 50 ng of vitamin D too high, just right, or not enough
Publisher wants $36 for the PDF
2 charts from Google images
Background & aims: Vitamin D impairs tumour-related transformation and supports the anticancer function of the immune system. Currently, there are no guidelines on vitamin D supplementation devoted solely to cancer patients. The primary objective of the study was to evaluate the frequency of vitamin D deficiency in Caucasian cancer patients and to characterize the clinical factors that predispose individuals to decreased vitamin D concentration. Secondly, the study aimed to estimate the dose of vitamin D supplementation that would prevent deficiencies in patients with cancer.
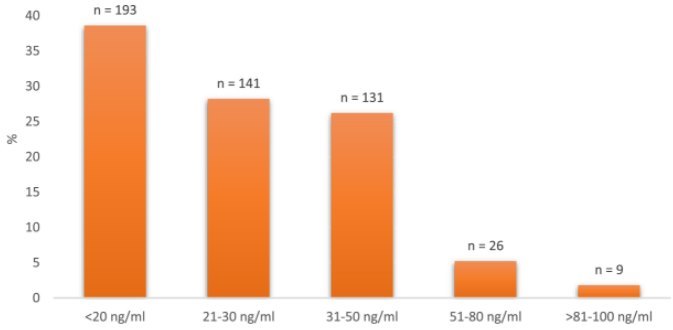
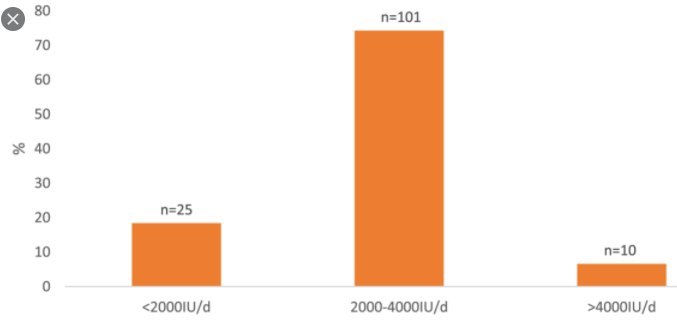
Methods: In the presented cross-sectional study the population consisted of 500 consecutive Caucasian patients with a diagnosis of neoplastic disease, some of which declared long-term vitamin D supplementation in various doses. Serum vitamin D concentration was measured once in all patients and clinical data were obtained from the hospital database. The frequencies of vitamin D deficiency were compared to certain clinical variables by appropriate statistical tests. The dose of vitamin D substitution in cancer patients was estimated using the receiver operating characteristic (ROC) curve.
Results: Vitamin D deficiency was diagnosed in 66.8% of patients with cancer and even in 31.6% who declared vitamin D supplementation. Older age, male gender, diagnosis of head and neck cancer or squamous cell carcinoma and body mass loss were identified as factors that predispose to vitamin D deficiency. The dose of vitamin D that would prevent deficiency in Caucasian patients with cancer was set at 2250 IU daily.
Conclusions: Vitamin D deficiency was very common in Caucasian patients with cancer, even in terms of vitamin D supplementation. The greatest predisposition was related to elder age, male gender, diagnosis of head and neck or squamous cell carcinoma and body mass loss. The dose of vitamin D supplementation in cancer patients should probably be higher than in the general population.
References
Vitamin D supplementation for extraskeletal indications in older persons. J Am Med Dir Assoc. 2020; 21: 164-171
Vitamin D: metabolism, molecular mechanism of action, and pleiotropic effects. Physiol Rev. 2015; 96: 365-408
Can we accurately measure the concentration of clinically relevant vitamin D metabolites in the circulation? The problems and their consequences. Endokrynol Pol. 2013; 64: 238-245
The role of vitamin D in reducing cancer risk and progression. Nat Rev Canc. 2014; 14: 342-357
The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord. 2017; 18: 153-165
The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of medicine: what clinicians need to know. J Clin Endocrinol Metabol. 2011 1; 96: 53-58
Practical guidelines for the supplementation of vitamin D and the treatment of deficits in Central Europe - recommended vitamin D intakes in the general population and groups at risk of vitamin D deficiency. vol. 64. Endokrynologia Polska, Poland2013: 319-327
Association of intestinal permeability with admission vitamin D deficiency in patients who are critically ill. J Invest Med. 2020; 68: 397-402
Vitamin D supplementation and total cancer incidence and mortality: a meta-Analysis of randomized controlled trials. Ann Oncol. 2019; 30 https://doi.org/10.1093/annonc/mdz059
The role of vitamin D and VDR in carcinogenesis: through epidemiology and basic sciences. J Steroid Biochem Mol Biol. 2017; 167: 203-218
Vitamin D and immunomodulation: is it time to change the reference values?. ACLS (Ann Clin Lab Sci). 2017; 47: 508-510
Vitamin D deficiency 2.0: an update on the current status worldwide. ur J Clin Nutr. 2020; 74: 1498-1513
Review of recent advances in understanding the role of Vitamin D in reducing cancer risk: breast, colorectal, prostate, and overall cancer. Anticancer Res. 2020; 40: 491-499
Vitamin D supplements and prevention of cancer and cardiovascular disease. N Engl J Med. 2019 Jan; 380: 33-44
Vitamin D supplementation guidelines. J Steroid Biochem Mol Biol. 2018; 175: 125-135
Vitamin D: an overview of vitamin D status and intake in Europe. Nutr Bull. 2014; 39: 322-350
Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009; 19 (2008/03/10): 73-78
Clinical outcomes of vitamin D deficiency and supplementation in cancer patients. Nutr Rev. 2013; 71: 611-621
Vitamin D deficiency in cancer patients and predictors for screening (D-ONC study). Curr Probl Canc. 2019; 43: 421-428
Comparison of vitamin D levels between healthy individuals and cancer patients. Eurasian J Med Invest. 2020; 4: 259-264
Vitamin D in head and neck cancer: a systematic review. Curr Oncol Rep. 2021; 23
Vitamin D deficiency in head and neck cancer patients–prevalence, prognostic value and impact on immune function. OncoImmunology. 2018; 7: 1-10
Circulating vitamin D in relation to cancer incidence and survival of the head and neck and oesophagus in the EPIC cohort. Sci Rep. 2016; 6: 36017
High prevalence of vitamin D deficiency in women with breast cancer: the first Chilean study. Breast. 2016; 29: 39-43
Vitamin D intake, blood vitamin D levels, and the risk of breast cancer: a dose-response meta-analysis of observational studies. Aging. 2019; 11: 12708-12732
Circulating vitamin D concentration and risk of seven cancers: mendelian randomisation study. BMJ (Clinical Research Ed). 2017; 359: j4761
Effects of vitamin D use on health-related quality of life of breast cancer patients in early survivorship. Integr Canc Ther. 2019; 18
- etc.
