5,000 IU Vitamin D daily resulted in many benefits after 3 months (US soldiers) – RCT
A Prospective Cohort Study of Vitamin D Supplementation in AD Soldiers: Preliminary Findings.
Mil Med. 2019 Mar 1;184(Suppl 1):498-505. doi: 10.1093/milmed/usy393.
McCarthy MS1, Elshaw EB2, Szekely BM2, Raju D3.
 * *📄 Download the PDF from Vitamin D Life* * Military* Military and Vitamin D - many studies* Trial starting for Vitamin D with US soldiers – 2,000 and 5,000 IU for 3 months – Nov 2016* Previous publication about this RCT - many problems noted at the time* Need for Routine Vitamin D Screening in Military Personnel – Sept 2016* US Army learning about benefits of vitamin D to trauma – Matthews Dec 2013 talking with Dr. Matthews* Huge increase in Vitamin D supplementation in the US military (2005-13) – Oct 2016Many months for Vitamin D level response, and even more for the body to get the benefits* Respond to daily Vitamin D in 2-12 months* Vitamin D response time is 3-6 months, not much benefit in first 4 months – RCT July 2017* 3 to 6 months to plateau with 4,000 IU vitamin D daily (Cardiac Patients) – June 2017
* *📄 Download the PDF from Vitamin D Life* * Military* Military and Vitamin D - many studies* Trial starting for Vitamin D with US soldiers – 2,000 and 5,000 IU for 3 months – Nov 2016* Previous publication about this RCT - many problems noted at the time* Need for Routine Vitamin D Screening in Military Personnel – Sept 2016* US Army learning about benefits of vitamin D to trauma – Matthews Dec 2013 talking with Dr. Matthews* Huge increase in Vitamin D supplementation in the US military (2005-13) – Oct 2016Many months for Vitamin D level response, and even more for the body to get the benefits* Respond to daily Vitamin D in 2-12 months* Vitamin D response time is 3-6 months, not much benefit in first 4 months – RCT July 2017* 3 to 6 months to plateau with 4,000 IU vitamin D daily (Cardiac Patients) – June 2017📄 Download the PDF from Vitamin D Life
PURPOSE: To explore response to vitamin D supplementation in active duty (AD) warfighters and translate findings into evidence-based health policy.
BACKGROUND: Soldiers are at risk for musculoskeletal injuries and metabolic dysfunction that impact physical performance and military readiness; the link with low vitamin D status is unclear.
METHODS:
This prospective trial enrolled 152 soldiers; baseline 25 hydroxyvitamin (OH) D level determined assignment to a no-treatment control (CG) or treatment group (TG) receiving a vitamin D3 supplement for 90 days. Symptoms, diet, sun exposure, and blood biomarkers obtained at baseline (T1) and 3 months (T2).
RESULTS:
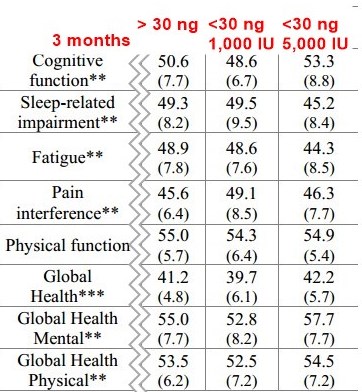
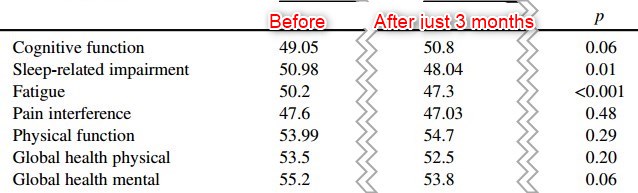
Cohort was predominantly white (58%) with a significant difference in racial distribution for vitamin D status. Mean (SD) 25(OH)D levels were 37.8 (5.6) ng/mL, 22.2 (5.0) ng/mL, and 22.9 (4.7) ng/mL for the CG, low dose TG, and high-dose TG at T1, respectively. Following three months of treatment, one-way ANOVA indicated a statistically significant difference between groups (F5,246 = 44.37; p < 0.0001). Vitamin D intake was 44% of Recommended Dietary Allowance throughout the first phase of the trial. Patient-Reported Outcomes Measurement Information System scores improved in TG for fatigue and sleep, p < 0.01.
CONCLUSIONS: Vitamin D deficiency is widespread in AD soldiers. Clinicians must intervene early in preventable health conditions impacting warfighter performance and readiness and recommend appropriate self-care strategies.
