400,000 IU of Vitamin D before surgery should cost-effectively reduce infection after knee replacement
Preoperative Vitamin D Repletion in Total Knee Arthroplasty: A Cost-Effectiveness Model
The Journal of Arthroplasty Volume 35, Issue 5, May 2020, Pages 1379-1383 https://doi.org/10.1016/j.arth.2019.12.037
50,000 IU of vitamin D weekly for 8 weeks cut the infection rate in half
Background
Recent studies have identified vitamin D deficiency (serum 25-hydroxyvitamin D [25(OH)D] < 20 ng/L) as a potentially modifiable risk factor for prosthetic joint infection (PJI) in arthroplasty. The purpose of this study is to determine whether implementation of preoperative 25(OH)D repletion is cost-effective for reducing PJI following total knee arthroplasty (TKA).
Methods
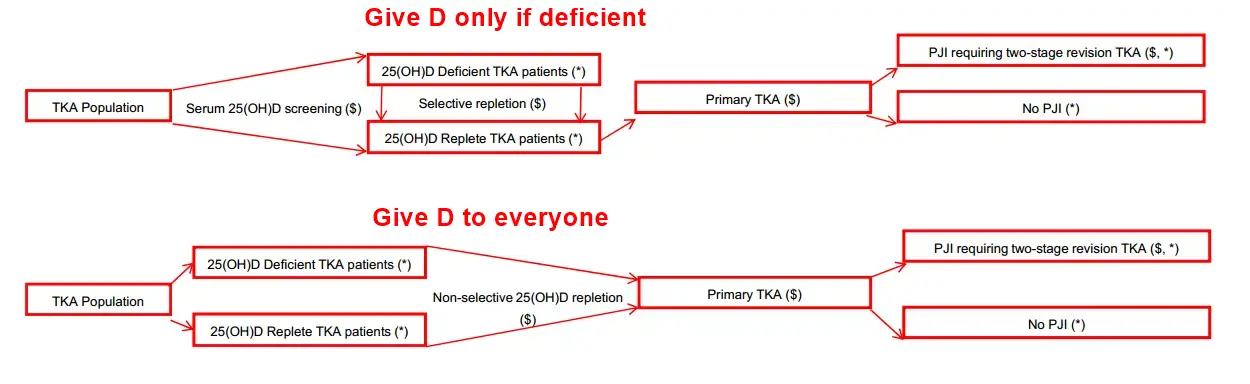
A cost estimation predictive model was generated to determine the utility of both selective and nonselective 25(OH)D repletion in primary TKA to prevent PJI. Input data on the incidence of 25(OH)D deficiency, relative complication rates, and costs of serum 25(OH)D repletion and 2-stage revision for PJI were derived from previously published literature identified using systematic review and publicly available data from Medicare reimbursement schedules. Mean, lower, and upper bounds of 1-year cost savings were computed for nonselective and selective repletion relative to no repletion.
Results
Selective preoperative 25(OH)D screening and repletion were projected to result in $1,504,857 (range, $215,084-$4,256,388) in cost savings per 10,000 cases. Nonselective 25(OH)D repletion was projected to result in $1,906,077 (range, $616,304-$4,657,608) in cost savings per 10,000 cases. With univariate adjustment, nonselective repletion is projected to be cost-effective in scenarios where revision for PJI costs ≥$10,636, incidence of deficiency is ≥1.1%, and when repletion has a relative risk reduction ≥4.2%.
Conclusion
This predictive model supports the potential role of 25(OH)D repletion as a cost-effective mechanism of reducing PJI risk in TKA. Given the low cost of 25(OH)D repletion relative to serum laboratory testing, nonselective repletion appears to be more cost-effective than selective repletion. Further prospective investigation to assess this modifiable risk factor is warranted.
Thus: Save $190 / patient ($1.9 million cost reductions in later infections if give vitamin D to all 10,000 patients)
📄 Download the PDF from Sci-Hub via Vitamin D Life
Loading dose lasts about 3 months - should have followed up with 50,000 IU bi-weekly
Note: Study does not consider larger savings due to: recovery weeks faster, decreased need for physical therapy
Note: My wife is quickly recovering from knee replacement surgery in late Oct 2024
I had given her 400,000 IU sublingual nanoemulsion vitamin D 1 week before her surgery
And also applied about 20,000 IU of Vitamin D topically near to her cut on a weekly basis.
Note: Her normal vitamin D level is > 100 ng/mL
We also used Earthing
About 1% TKA infections ==> 230,000/year by 2030
Vitamin D Life – Vitamin D is needed before many surgeries – many studies and RCTs contains
{include}
High-Dose Vitamin D Supplementation Can Correct Hypovitaminosis D Prior to Total Knee Arthroplasty - Feb 2022
The Journal of Arthroplasty Volume 37, Issue 2, February 2022, Pages 274-278 https://doi.org/10.1016/j.arth.2021.10.016
loading dose of 50,000 IU D3 weekly for 4 weeks then 2000 IU/d.
"Vitamin D deficiency in THA and TKA patients has been associated with inferior surgical outcomes, increased risk of complications, and longer postoperative length of stay"
Vitamin D improves Total Knee Arthroplasty - Meta-analysis April 2024
Vitamin D Deficiency Leads to Poorer Health Outcomes and Greater Length of Stay After Total Knee Arthroplasty and Supplementation Improves Outcomes - A Systematic Review and Meta-Analysis
JBJS Reviews 12(4):e23.00150, April 2024. | DOI: 10.2106/JBJS.RVW.23.00150
Vivek, Kavyesh BSc (Hons)1; Kamal, Rayan BSc (Hons)1; Perera, Edward BSc, MBBS2; Gupte, Chinmay M. PhD, FRCS(Tr&Orth;), MA, BMBCh (Oxon)1,2,a
Background:
Vitamin D deficiency is increasingly identified as a predictor of poorer outcomes in musculoskeletal disease affecting as many as 1 in 4 people. This study aimed to evaluate the effect of vitamin D supplementation on outcomes after primary total knee arthroplasty (TKA).
Methods:
A targeted search of terms related to vitamin D and TKA outcomes was performed in PubMed, Cochrane Central Register of Controlled Trials, ClinicalTrials.gov, American Academy of Orthopaedic Surgeons, and British Orthopaedic Association databases. The results were analyzed using forest plots with I2 heterogeneity statistics and pooled effects with 95% confidence intervals (CIs) and p values. A p < 0.05 was considered statistically significant.
Results:
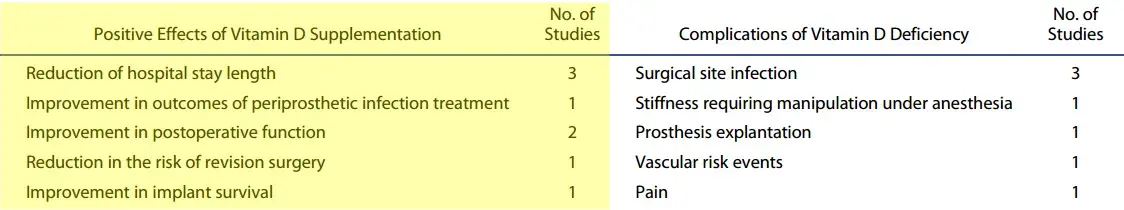
A total of 146,054 patients with 150,107 TKRs were analyzed in 10 studies that complied with the inclusion criteria, of which 3 were suitable for meta-analysis. Of these, 4 of the 10 studies showed that vitamin D deficiency resulted in poorer functional outcome scores (Western Ontario and McMasters Universities Osteoarthritis Index, Knee Society Scoring System, and American Knee Society scores), as well as increased risk of revision surgery, incidence of joint infection, and postoperative stiffness. Meta-analysis of length of hospital stay (LOS) demonstrated a significant increase in LOS in patients with vitamin D deficiency (standardized mean difference, −0.54, 95% CI, −0.69 to −0.38, p < 0.00001). Furthermore, outcomes were improved with vitamin D supplementation in 6 of 10 studies.
Conclusion:
Vitamin D deficiency results in poorer outcomes of primary TKA, with improved outcomes after supplementation. Further studies should examine the role of preoperative vitamin D screening and/or perioperative supplementation in primary TKA and standardize outcome measures to assess their effect.
📄 Download the PDF from Vitamin D Life
Vitamin D before lumbar fusion saved $198 per surgery - Feb 2023
Vitamin D supplementation is a cost-effective intervention after posterolateral lumbar fusion: a systematic review
Current Orthopaedic Practice 34(1):p 9-15, January/February 2023. DOI: 10.1097/BCO.0000000000001188 PDF behind paywall
Patel, Dhiraj BA; Lippel, Matthew BA; Lunardini, David MD; Monsey, Robert MD; Ziino, Chason MD
