Overview Schizophrenia and Vitamin D
15 reasons to think that schizophrenia is associated with low vitamin D
1) 97% of patients with schizophrenia are vitamin D deficient
2) Schizophrenia varies with latitude (UVB) by 10X (controversy)
3) Schizophrenia is more common in those with dark skin (when away from the equator)
4) Schizophrenia is associated with low natal vitamin D
5) Schizophrenia has been increasing around the world when vitamin D has been decreasing (controversy)
6) Schizophrenia is associated with low birth rate, which is associated with low vitamin D
7) Schizophrenia is associated with Autism which is associated with low vitamin D
8) Schizophrenia Bulletin Editorial (Jan 2014) speculated that Vitamin D could be a major player
9) Schizophrenia 2X more likely if low vitamin D - meta-analysis
10) Schizophrenia increased 40 % for Spring births after Danes stopped vitamin D fortification
11) Schizophrenia is associated with season of birth
12) Schizophrenia is associated with poor Vitamin D Receptor genes
13) Schizophrenia risk is decreased if give Vitamin D after birth
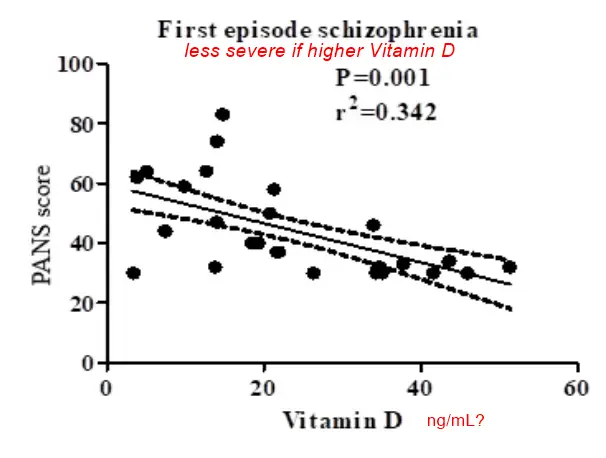
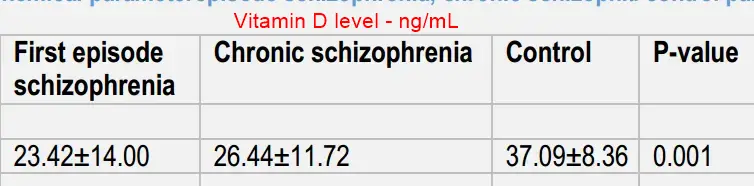
14) Schizophrenia - first episode symptoms are worse if low Vitamin D
15) Schizophrenia symptoms reduced when Vitamin D levels are restored
Omega-3 may treat schizophrenia wonder if Omega-3 and Vitamin D would be additive or even synergistic
32+ Vitamin D Life pages have SCHIZOPHRENIA in the title
The list is automatically updated
{LIST()}
The many associations of Schizophrenia with Vitamin D - Perplexity AI Report May 2025
See also Vitamin D Life
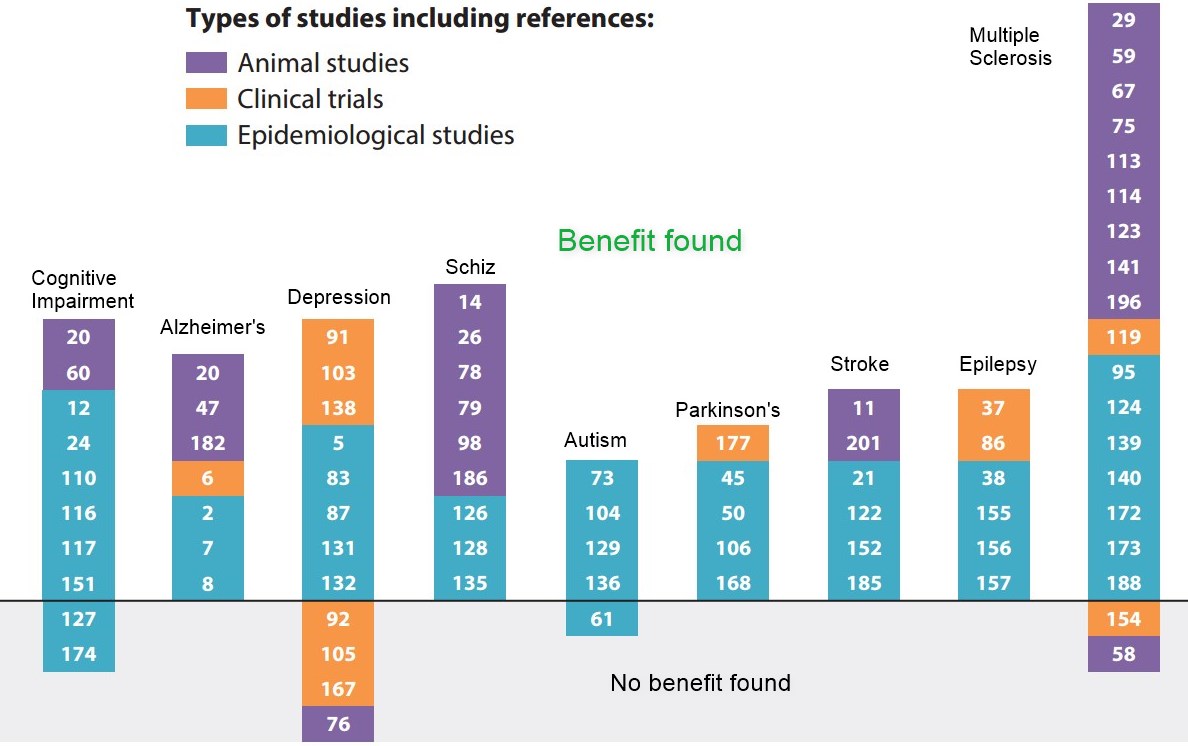
- Schizophrenia and vitamin D have latitude-related genes – Nov 2010 which has the following graphic
Omega-3 and Schizophrenia
Psychosis risk reduced for 80 weeks by just 12 weeks of Omega-3 – RCT Aug 2017
Violent schizophrenia patients treated by 3 months of Omega-3 – RCT Aug 2017
Schizophrenia relapses reduced 3X by Omega-3 – RCT Mar 2015
B12 and Schizophrenia
Autistics and Schizophrenics have 3X lower Vitamin B12 levels in the brain – Jan 2016
Schizophrenia might be treated by folic acid, vitamin B12 and vitamin D – May 2014
Pages in both of the categories of Intervention AND Cognitive
{category}
Schizophrenia - first episode symptoms are less severe if higher Vitamin D - April 2025
📄 Download the PDF from Vitamin D Life
Schizophrenia associated with anxiety, bipolar, and suicide - MR analysis April 2023
Schizophrenia and co-morbidity risk: Evidence from a data-driven phenome-wide association study
J Psychiatr Res. 2023 Apr 10;162:1-10. doi: 10.1016/j.jpsychires.2023.04.010 PDF is behind a paywall
Anwar Mlugeta 1, Vijayaprakash Suppiah 2, Elina Hyppönen 3
Schizophrenia is a chronic debilitating psychiatric disorder with significant morbidity and mortality. In this study, we used information from 337,484 UK Biobank participants and performed PheWAS using schizophrenia genetic risk score on 1135 disease outcomes. Signals that passed the false discovery rate threshold were further analyzed for evidence of the causality of the association. We extended the analysis to 30 serum, four urine, and six neuroimaging biomarkers to identify biomarkers that could be affected by schizophrenia. Schizophrenia GRS was associated with 54 (39 distinct) disease outcomes, including schizophrenia in the PheWAS analysis.
Of these, a causal association were found with 10 distinct diseases in the MR analysis.
Schizophrenia is causally linked with higher odds of
anxiety (OR = 1.41, 95%CI 1.12 to 1.21),
bipolar disorder (OR = 1.52, 95%CI 1.36 to 1.70),
major depressive disorder (OR = 1.12, 95%CI 1.08 to 1.16) and
suicidal ideation (OR = 1.30, 95%CI 1.19 to 1.42).
Lower odds were found for several diseases including type 1 diabetes, coronary atherosclerosis and some musculoskeletal disorders. In analyses using biomarkers, schizophrenia was associated with lower serum 25(OH)D, gamma glutamyltransferase, cystatin C, serum creatinine. However, we did not find association with any of the brain imaging markers. Our analyses confirmed the co-existence of schizophrenia with other mental health disorders but did not otherwise suggest strong effects on disease risk. Biomarker analyses reflected associations which could be explained by unhealthy lifestyles, suggesting patients with schizophrenia may benefit from screening for and managing broader health aspects.
2 related mental health studies
Season of birth increased risk of Schizophrenia by 5% - Meta-analysis Feb 2023
Systematic review and meta-analysis: Season of birth and schizophrenia risk
Schizophrenia Research Volume 252, February 2023, Pages 244-252 https://doi.org/10.1016/j.schres.2022.12.016
Samantha M. Coury a, Adam Lombroso a, Victor J. Avila-Quintero a, Jerome H. Taylor b c, José M. Flores a d 1, Natalia Szejko e f, Michael H. Bloch a d
Objective
Winter birth has been hypothesized to be associated with increased schizophrenia risk for nearly a century. Major hypotheses regarding the potential etiological risk factors for schizophrenia such as vitamin D deficiency and virus exposure in utero are predicated based on the observation that risk of schizophrenia is higher in children born in winter months.
Methods
We conducted a systematic review and meta-analysis to examine the association between season and month of birth and risk of schizophrenia. We further investigated this relationship stratified by hemisphere.
Results
Forty-three studies spanning 30 countries and territories and 440,039 individuals with schizophrenia were included in this meta-analysis. Winter births were associated with a small but statistically significant increased risk of schizophrenia (OR 1.05, 95 % CI 1.03–1.07, p < 0.0001) and summer births were associated with a small but statistically significant decreased risk of schizophrenia (OR 0.96, 95 % CI 0.94–0.98, p = 0.0001). Stratified subgroup analysis demonstrated no significant difference between hemispheres in the risk of schizophrenia for either winter or summer births.
Conclusions
Analysis using birth month data demonstrated a clear seasonal trend towards increased risk of schizophrenia being associated with winter birth months and decreased risk of schizophrenia in summer-to-fall months in the Northern but not Southern Hemisphere. These data suggest a small-but-substantial increased risk of schizophrenia in winter birth month. Further research needs to examine potential etiologic causes for this association.
Prenatal Vitamin D might decrease Schizophrenia incidence by 30% - 2019
📄 Download the PDF from Vitamin D Life
NAC treats Schizophrenia slightly better than vitamin D (review of 17 RCT) – May 2022
The efficacy of nutritional supplements for the adjunctive treatment of schizophrenia in adults: A systematic review and network meta-analysis
Psychiatry Research, May 2022, https://doi.org/10.1016/j.psychres.2022.114500 $36 paywall
XianrongXua#GeShaoab#XuZhangaYanHuaJiaHuangcYousongSucMinZhangcYiyunCaidHuipingZhoue
Highlights
Compared with placebo, N-acetyl cysteine supplement was associated with a significant reduction in PANSS score in schizophrenia patients, but this association was not found in schizophrenia patients treated with folic acid or vitamin B12, omega-3 polyunsaturated fatty acid and vitamin D.
The results from network meta-analysis indicated that N-acetyl cysteine supplement was significantly more efficacious than folic acid or vitamin B12 and omega-3 polyunsaturated fatty acid in the term of PANSS score changes.
The estimated ranking probabilities of treatments showed that NAC might be the most effective intervention overall nutritional supplements.
Nutritional supplementations have been widely used as adjunctive treatments for schizophrenia. However, among these supplementations, of which the most beneficial is currently unknown. This study aimed to compare and rank the effectiveness of nutritional supplementations in the adjunctive treatments of schizophrenia. The four nutritional supplementations evaluated were:
1) folate acid or vitamin B12;
2) vitamin D;
3) N-acetyl cysteine (NAC);
4) Omega-3 polyunsaturated fatty acid, including docosahexaenoic acid (DHA)
- and eicosapentaenoic acid (EPA).
17 eligible RCTs with 1165 participants were included in this network meta-analysis based on study criteria. NAC supplementation was significantly more efficacious than folic acid or vitamin B12 [MD (95% CI): −6.6 (−10.8, −2.4)] and omega-3 polyunsaturated fatty acid [MD (95% CI): –5.1(−9.9, -0.8)] supplementation in the term of PANSS score changes.
There were no significant differences in the PANSS score changes between NAC and vitamin D [MD (95% CI): −5.2 (−10.9, 0.5)] supplementations . The estimated ranking probabilities of treatments showed that NAC might be the most effective adjunctive intervention overall nutritional supplementations. These results indicate that NAC could improve PANSS score and it may be among the most effective nutritional supplementations in schizophrenia patients.
Schizophrenia and COVID-19 - March 2021
- 1.3 X for Schizophrenia
3X more likely to die of COVID-19 if Schizophrenic Sept 2021
Low vitamin D in early life may be associated with Schizophrenia, need more evidence - July 2021
Developmental exposure to vitamin D deficiency and subsequent risk of schizophrenia
Schizophr Res. 2021 Jul 8;S0920-9964(21)00216-4. doi: 10.1016/j.schres.2021.06.004
Clara Albiñana 1, Sanne Grundvad Boelt 2, Arieh S Cohen 2, Zhihong Zhu 3, Katherine L Musliner 1, Bjarni J Vilhjálmsson 4, John J McGrath 5
Over the last half-century, a body of convergent evidence has accumulated linking disruption of early brain development with an increased risk of mental disorders, including schizophrenia. The orderly cascade of brain development may be disrupted by exposure to suboptimal concentrations of a range of biological substrates and micronutrients. We hypothesized that those exposed to vitamin D deficiency during early life have an increased risk of neurodevelopmental disorders, including schizophrenia. The hypothesis was based on the link between an increased risk of schizophrenia in (a) those born in winter and spring, when vitamin D deficiency is more prevalent, and (b) the offspring of dark-skinned migrants living in cold climates, who have a markedly increased risk of vitamin D deficiency.
In this review, we summarize evidence from analytic epidemiology related to this hypothesis. Two case-control studies based on Danish neonatal dried blood spots have found that neonatal vitamin deficiency is associated with an increased risk of schizophrenia. However, recent genetic analyses have also suggested that common variants linked to schizophrenia may lead to lower vitamin D concentrations (possibly mediated via reduced outdoor activity). We summarize the limitations of the current evidence and outline suggestions that can guide future research. Based on currently available data, there is insufficient evidence to support public health recommendations related to this topic.
However, we cannot reject the hypothesis that the provision of vitamin D supplementation to pregnant women and/or offspring in groups vulnerable to vitamin D deficiency may subsequently reduce the incidence of schizophrenia in the offspring.
📄 Download the PDF from Vitamin D Life
The Relationship between Symptom Severity and Low Vitamin D Levels in Patients with Schizophrenia.- Oct 2016
PLoS One. 2016 Oct 27;11(10):e0165284. doi: 10.1371/journal.pone.0165284. eCollection 2016.
Doğan Bulut S1, Bulut S2, Görkem Atalan D3, Berkol T4, Gürçay E5, Türker T6, Aydemir Ç7.
BACKGROUND:
In recent years, the relationship between schizophrenia and environmental factors has come into prominence. This study investigated the relationship between vitamin D levels and the positive and negative symptoms of schizophrenia by comparing vitamin D levels between patients with schizophrenia and a healthy control group.
METHODS:
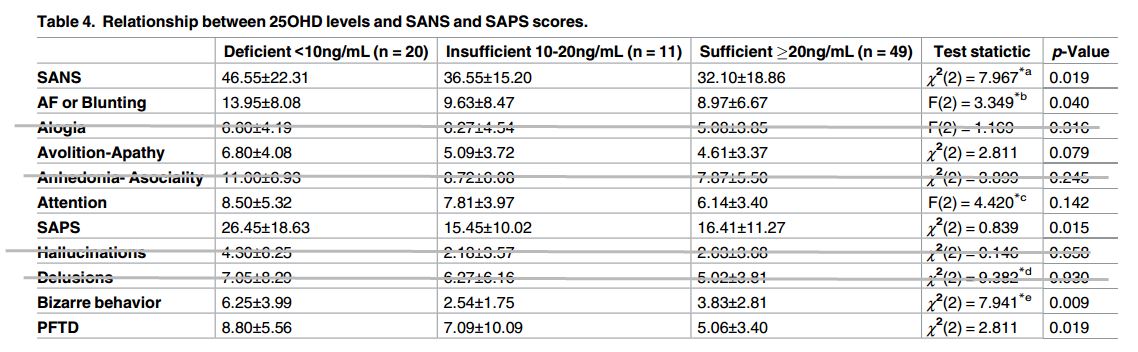
The study included 80 patients diagnosed with schizophrenia and 74 age- and sex-matched controls. The Scale for the Assessment of Negative Symptoms (SANS) and the Scale for the Assessment of Positive Symptoms (SAPS) were used to evaluate symptom severity. The 25-hydroxyvitamin D (25OHD) levels of all subjects both patients and healthy controls were analyzed in relation to measurements of symptom severity.
RESULTS:
There were no significant differences between the groups in terms of age, sex, or physical activity. Their mean 25OHD levels were also similar (23.46±13.98ng/mL for the patient group and 23.69±9.61ng/mL for the control group).
But when patients with schizophrenia were grouped based on their vitamin D levels, the results indicated statistically significant differences between their vitamin D levels and their
total SANS,
affective flattening, and
total SAPS,
bizarre behavior and
positive formal thought disorder scores
(p = 0.019, p = 0.004, p = 0.015, p = 0.009 and p = 0.019, respectively).
There is a negative correlation between 25OHD levels and SANS total points (r = -0.232, p = 0.038); a negative correlation for attention points (r = -0.227, p = 0.044) and negative correlation with positive formal thoughts (r = -0.257, p = 0.021).
CONCLUSION:
The results of this study show a relationship between lower levels of vitamin D and the occurrence of positive and negative symptoms, along with increased severity of symptoms at lower levels of vitamin D, suggesting that treatment for schizophrenia should include assessment of patients' vitamin D levels. We recommend that patients with schizophrenia should be assessed with regard to their vitamin D levels.
📄 Download the PDF from Vitamin D Life
Vitamin D Council descripiton of this study
Clipped from Discussion
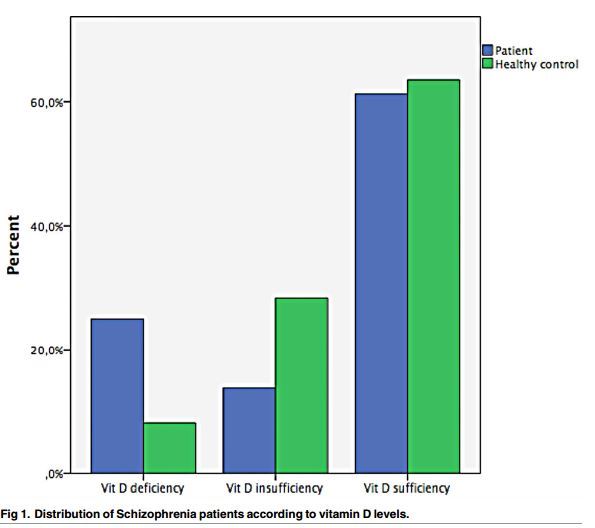
Of the schizophrenia patients who participated in our study,
20% showed deficient levels of vitamin D;
13.75% were found to have insufficient levels; and
61.25% were found to have sufficient levels.
The healthy controls in our study showed 8.1% deficient, 28.4% insufficient and 63.5% sufficient levels of Vitamin D. Although the deficient percentage among the schizophrenia patients was higher, the levels found for vitamin D in our schizophrenia patients and healthy controls was not statistically significant.
– – – –
The differing results obtained in these studies could be the result of factors like darker complexions and geographic differences in where the studies were conducted .
Other factors may also make a difference for instance differences in phases of the disorder like acute or chronic stages. Also differences were observed between patients experiencing acute exacerbation and those in remission.
Greater levels of negative and positive symptoms may
increase nutritional problems,
reduce the amount of exposure to sunlight, and
encourage more sedentary lifestyle habits.
This may also account for lower levels of vitamin D in patients undergoing acute episodes of schizophrenia when compared with more similar levels in those in remission and in controls. It is also possible that the different scores could be a result of taking blood samples during different seasons of the year. Studies done by Graham et al. and Yuksel et al. [16,17] like ours, took care to gather blood samples during the same season. This could be a reason for the similar results obtained by our study and these others.
– – – – –
Associations between Vitamin D deficiency and obesity, smoking, and lack of physical activity have been shown in previous studies [40-43] and we analyzed those variables in the current study as well. Although there were significant differences between healthy controls and our patient group in terms of obesity and smoking, there was no statistically significant difference in their vitamin D values. Our study did not look carefully at nutrition and patients who took supplemental vitamin D. We know that, other than supplements, sunlight exposure is the primary source of vitamin D for the majority of people [44]. In our study, the similarity of vitamin D levels, despite large statistical differences between our schizophrenia patient group and controls in relation to smoking and obesity, supports the idea that sunlight is a very important factor. When patients with schizophrenia were grouped according to their levels of vitamin D deficiency, there were no statistically significant differences in terms of obesity and smoking between the groups. This finding strengthens the finding of a relationship between vitamin D deficiency and symptom severity.
Schizophreniform and Autism Spectrum Syndromes: both had very low levels of Vitamin D - Oct 2016
Vitamin D Deficiency in Adult Patients with Schizophreniform and Autism Spectrum Syndromes: A One-Year Cohort Study at a German Tertiary Care Hospital.
Front Psychiatry. 2016 Oct 6;7:168. eCollection 2016.
Endres D1, Dersch R2, Stich O2, Buchwald A3, Perlov E1, Feige B1, Maier S1, Riedel A1, van Elst LT1.
INTRODUCTION:
Vitamin D has many immunomodulatory, anti-inflammatory, and neuroprotective functions, and previous studies have demonstrated an association between vitamin D deficiency and neuropsychiatric disease. The aim of our study was to analyze the prevalence of vitamin D deficiency in a 1-year cohort of adult inpatients with schizophreniform and autism spectrum syndromes in a naturalistic inpatient setting in Germany.
PARTICIPANTS AND METHODS:
Our study was comprised of 60 adult schizophreniform and 23 adult high-functioning autism spectrum patients who were hospitalized between January and December of 2015. We compared our findings with a historical German reference cohort of 3,917 adults using Pearson's two-sided chi-squared test. The laboratory measurements of 25-hydroxyvitamin D2/3 [25(OH)vitamin D] were obtained using a chemiluminescence immunoassay.
RESULTS:
In the schizophreniform group, we found decreased (<20 ng/ml) 25(OH)vitamin D levels in 48/60 (80.0%) of the patients.
In the autism spectrum group, decreased levels were detected in 18/23 (78.3%) of the patients.
25(OH)vitamin D deficiencies were found in 57.3% of the historical control group.
Particularly, severe deficiencies (<10 ng/ml) occurred much more frequently in the schizophreniform (38.3%) and autism spectrum groups (52.2%),
when compared to the control group (16.3%).
The recommended 25(OH)vitamin D values of >30 ng/ml were observed in only 5% of the schizophreniform patients, 8.7% of the autism spectrum patients, and 21.9% of the healthy controls.
DISCUSSION:
We found very high rates of 25(OH)vitamin D deficiencies in both patient groups and have discussed whether our findings might be related to alterations in the immunological mechanisms. Irrespective of the possible pathophysiological links between vitamin D deficiency and schizophrenia or autism spectrum disorders, more frequent measurement of vitamin D levels seems to be justified in these patient groups. Further prospective, controlled, blinded, and randomized research should be conducted to analyze the effectiveness of vitamin D supplementation on the improvement of psychiatric symptoms.
DOI: 10.3389/fpsyt.2016.00168 full free PDF online
Association between serum levels of bioavailable vitamin D and negative symptoms in first-episode psychosis - Sept 2016
Psychiatry Res. 2016 Sep 30;243:390-4. doi: 10.1016/j.psychres.2016.07.003
Yee JY1, See YM2, Abdul Rashid NA2, Neelamekam S2, Lee J3.
1 Research Division, Institute of Mental Health, Singapore. jieyin[email protected].
2 Research Division, Institute of Mental Health, Singapore.
3Office of Clinical Sciences, Duke-NUS Graduate Medical School, Singapore; Department of General Psychiatry 1, Institute of Mental Health, Singapore.
Total vitamin D levels had been commonly reported to be lowered in patients with chronic psychotic illnesses in countries from the higher latitudes. However, studies on patients with first-episode psychosis (FEP) are limited. In this study we investigated serum concentrations of total and bioavailable vitamin D levels in FEP patients compared to healthy controls and the association between symptom severity and vitamin D components. A total of 31 FEP patients and 31 healthy controls were recruited from Institute of Mental Health, Singapore. FEP patients were identified using Structured Clinical Interview for DSM-IV Axis I disorders (SCID-1) and severity symptoms were assessed using the positive and negative syndrome scale (PANSS). Sera from participants were analyzed for total vitamin D, vitamin D-binding protein (DBP) and bioavailable vitamin D. Linear regressions were performed to examine the associations between serum total and bioavailable vitamin D and the PANSS subscales. Current study noted a significantly lower bioavailable vitamin D was in the FEP group and an association between bioavailable vitamin D and negative symptoms in FEP patients in a population with a consistent supply of sun exposure throughout the year.
DOI: 10.1016/j.psychres.2016.07.003 Free PDF online
Low Vitamin D might be an effect rather than a cause of schizophrenia - May 2016
Note: This study considers vitamin D blood levels, not cell levels (3 genes can block cell levels and not be seen by blood tests)
Investigating causality in the association between 25(OH)D and schizophrenia
Sci Rep. 2016 May 24;6:26496. doi: 10.1038/srep26496.
Taylor AE1,2,3, Burgess S1,4, Ware JJ1,2,5, Gage SH1,2,3, Richards JB6,7,8, Davey Smith G1,5, Munafò MR1,2,3.
Vitamin D deficiency is associated with increased risk of schizophrenia. However, it is not known whether this association is causal or what the direction of causality is. We performed two sample bidirectional Mendelian randomization analysis using single nucleotide polymorphisms (SNPs) robustly associated with serum 25(OH)D to investigate the causal effect of 25(OH)D on risk of schizophrenia, and SNPs robustly associated with schizophrenia to investigate the causal effect of schizophrenia on 25(OH)D. We used summary data from genome-wide association studies and meta-analyses of schizophrenia and 25(OH)D to obtain betas and standard errors for the SNP-exposure and SNP-outcome associations. These were combined using inverse variance weighted fixed effects meta-analyses. In 34,241 schizophrenia cases and 45,604 controls, there was no clear evidence for a causal effect of 25(OH)D on schizophrenia risk. The odds ratio for schizophrenia per 10% increase in 25(OH)D conferred by the four 25(OH)D increasing SNPs was 0.992 (95% CI: 0.969 to 1.015). In up to 16,125 individuals with measured serum 25(OH)D, there was no clear evidence that genetic risk for schizophrenia causally lowers serum 25(OH)D. These findings suggest that associations between schizophrenia and serum 25(OH)D may not be causal. Therefore, vitamin D supplementation may not prevent schizophrenia.
PMID: 27215954 PMCID: PMC4877705 DOI: 10.1038/srep26496 📄 Download the PDF from Vitamin D Life
97% of Schizophrenia patients were vitamin D deficient, and associated small brain volumes - June 2015
Psychiatry Res. 2015 Jun 24. pii: S0925-4927(15)30013-5. doi: 10.1016/j.pscychresns.2015.06.006
Serum vitamin D and hippocampal gray matter volume in schizophrenia.
Shivakumar V1, Kalmady SV2, Amaresha AC2, Jose D2, Narayanaswamy JC2, Agarwal SM2, Joseph B2, Venkatasubramanian G3, Ravi V4, Keshavan MS5, Gangadhar BN6.
Disparate lines of evidence including epidemiological and case-control studies have increasingly implicated vitamin D in the pathogenesis of schizophrenia. Vitamin D deficiency can lead to dysfunction of the hippocampus - a brain region hypothesized to be critically involved in schizophrenia. In this study, we examined for potential association between serum vitamin D level and hippocampal gray matter volume in antipsychotic-naïve or antipsychotic-free schizophrenia patients (n=35). Serum vitamin D level was estimated using 25-OH vitamin D immunoassay. Optimized voxel-based morphometry was used to analyze 3-Tesla magnetic resonance imaging (MRI) (1-mm slice thickness). Ninety-seven percent of the schizophrenia patients (n=34) had sub-optimal levels of serum vitamin D (83%, deficiency; 14%, insufficiency).
A significant positive correlation was seen between vitamin D and regional gray matter volume in the right hippocampus after controlling for age, years of education and total intracranial volume (Montreal Neurological Institute (MNI) coordinates: x=35, y=-18, z=-8; t=4.34 pFWECorrected=0.018). These observations support a potential role of vitamin D deficiency in mediating hippocampal volume deficits, possibly through neurotrophic, neuroimmunomodulatory and glutamatergic effects.
Schizophrenia 2X more likely if low vitamin D - meta-analysis July 2014
Serum Vitamin D Levels in Relation to Schizophrenia: A Systematic Review and Meta-Analysis of Observational Studies.
J Clin Endocrinol Metab. 2014 Jul 22:jc20141887
Valipour G1, Saneei P, Esmaillzadeh A.
Introduction: Although several observational studies have investigated the association between vitamin D status and schizophrenia, we are aware of no comprehensive meta-analysis in this regard. Objective: We aimed to conduct a systematic review and a meta-analysis of observational studies to summarize the available data on the association between serum vitamin D levels and schizophrenia. Methods: A systematic research on all published articles until October 2013 was conducted in PubMed, ISI (Web of science), SCOPUS, and Google Scholar. All observational studies that had measured serum vitamin D levels in schizophrenic patients were included in the systematic review. After considering exclusion criteria, we had 19 studies for the systematic review that were included in three separate meta-analyses: 1) a meta-analysis on mean levels of 25-hydroxyvitamin D [25(OH)D] (n = 13); 2) a meta-analysis on the prevalence of vitamin D deficiency (n = 8); 3) a meta-analysis on odds ratios (n = 8). Results: Findings from a meta-analysis on means revealed that the overall mean difference in serum 25(OH)D levels between schizophrenic patients and control participants was -5.91 ng/mL [95% confidence interval (CI) -10.68, -1.14]. Subgroup analyses based on study design, the patient's hospitalization status, study quality, and study location did not explain between-study heterogeneity; however, type of biomarker assessed [25-dihydroxyvitamin D3 vs 25OH)D)] could account for some degree of heterogeneity. Results from the meta-analysis on the prevalence of vitamin D deficiency indicated that the overall prevalence of vitamin D deficiency in schizophrenic patients was 65.3% (95% CI 46.4%-84.2%).
Findings from the meta-analysis on odds ratios indicated that vitamin D-deficient persons were 2.16 times (95% CI 1.32, 3.56) more likely to have schizophrenia than those with vitamin D sufficiency. No evidence of heterogeneity was detected. Conclusion: We found a strong association between vitamin D deficiency and schizophrenia. However, randomized clinical trials are required to confirm our findings.

PDF is attached at the bottom of this page
Vitamin D Deficiency Doubles Risk of Developing Schizophrenia Vitamin D3 Blog Aug 2014
Review of the study, along with 2 short videos.
Related Clinical trials for TREATMENT
- Study of Vitamin D in the Severely Mentally Ill Clinical trial underway using 50,000 IU of vitamin D weekly for 3 months
- Would have greatly increased their chance of success if they had doubled both the dose and the time period, or had used a loading dose.
- 50,000 IU weekly, without a loading dose, will get some of the participants up to 40 nanograms of vitamin D by 3 months.
- Trial success would have been greater if they had a quick goal of >50 nanograms.
- Searched US clinical trials: (depressed OR depression OR schizophrenia OR psychotic OR psychosis OR autistic OR autism) "vitamin D" 191 interventions with vitamin D as of April 2023
- Vitamin D for Improving Metabolic Control and Depressive Symptoms (50,000 IU weekly)
- The Role of Vitamin D Supplementation on Well-Being and Symptoms of Depression During the Winter Season in Health Service Staff (2800 IU)
- Can Vitamin D3 Supplementation Affect Treatment Outcomes in Patients With Depression (2800 IU)
Psychotic are 3.5X more likely to be vitamin D deficient or have dark skin - 2012
Vitamin D deficiency and psychotic features in mentally ill adolescents: A cross-sectional study.
BMC Psychiatry. 2012 May 9;12(1):38.
Gracious BL, Finucane TL, Freidman-Campbell M, Messing S, Parkhurst MM.
BACKGROUND: Vitamin D deficiency is a re-emerging epidemic, especially in minority populations. Vitamin D is crucial not only for bone health but for proper brain development and functioning. Low levels of vitamin D are associated with depression, seasonal affective disorder, and schizophrenia in adults but little is known about vitamin D and mental health in the pediatric population.
METHODS: One hundred four adolescents presenting for acute mental health treatment over a 16-month period were assessed for vitamin D status and the relationship of 25-OH vitamin D levels to severity of illness, defined by presence of psychotic features.
RESULTS: Vitamin D deficiency (25-OH D levels <20 ng/ml) was present in 34%; vitamin D insufficiency (25-OH D levels 20-30 ng/ml) was present in 38%, with a remaining 28% in the normal range.
Adolescents with psychotic features had lower vitamin D levels (20.4 ng/ml vs. 24.7 ng/ml; p=0.04, 1 df).
The association for vitamin D deficiency and psychotic features was substantial (OR 3.5; 95% CI 1.4-8.9; p <0.009).
Race was independently associated with vitamin D deficiency and independently associated with psychosis for those who were Asian or biracial vs. white (OR=3.8; 95% CI 1.113.4; p<0.04). Race was no longer associated with psychosis when the results were adjusted for vitamin D levels.
CONCLUSIONS: Vitamin D deficiency and insufficiency are both highly prevalent in adolescents with severe mental illness. The preliminary associations between vitamin D deficiency and presence of psychotic features warrant further investigation as to whether vitamin D deficiency is a mediator of illness severity, result of illness severity, or both. Higher prevalence of vitamin D deficiency but no greater risk of psychosis in African Americans, if confirmed, may have special implications for health disparity and treatment outcome research.
#00F:CLICK HERE for PDF online
Association between first-episode schizophrenia and low vitamin D - Feb 2014, includes PDF
Relationship of low vitamin D status with positive, negative and cognitive symptom domains in people with first-episode schizophrenia.
Early Interv Psychiatry. 2014 Feb 24. doi: 10.1111/eip.12122.
Graham KA1, Keefe RS, Lieberman JA, Calikoglu AS, Lansing KM, Perkins DO.
AIM: Deficient vitamin D levels are very common among Americans of all ages and ethnicities, but little is known about its prevalence or associated problems among those with schizophrenia.
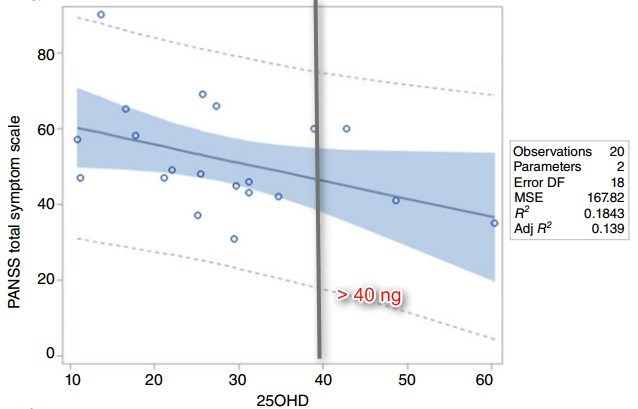
METHODS: Stored plasma from 20 recent onset schizophrenia subjects and 20 matched healthy comparison subjects were analysed for 25 OH vitamin D, and related to measures of symptom severity and neurocognition.
RESULTS: There was no significant difference in mean 25 OH vitamin D between the schizophrenia and the healthy comparison subjects (28.2 standard deviations (SD) 12.6 ng mL-1 vs. 29.9 SD 14.3 ng mL-1 ), and about half the subjects in each group had insufficient levels (<30 ng mL-1 ). Among psychosis subjects, greater severity of negative symptoms was correlated with lower vitamin D status (r = -0.55, P = 0.012); the correlations of overall symptom severity and positive symptom severity with 25 OH vitamin D levels approached significance (r = -0.42, P = 0.07 and r = -0.36, P = 0.12, respectively). There was no relationship of vitamin D with depressive symptoms. Among the schizophrenia subjects, lower 25 OH vitamin D levels were associated with more severe overall cognitive deficits (r = 0.56, P = 0.019).
CONCLUSION: This study found that lower vitamin D levels in schizophrenia subjects were associated with more severe negative symptoms and overall cognitive deficits. However, the cross-sectional design precludes any conclusions about whether low vitamin D status in fact causes more severe negative symptoms and cognitive impairments. No relationship was found between lower vitamin D levels and depressive symptoms.
Graph from attached PDF: 40 ng line added by Vitamin D Life
PDF is attached at the bottom of this page
Schizophrenia is related to many other diseases- many of which are associated with low vitamin D

Schizophrenics 6X more likely to be anxious if <10 ng of Vitamin D - Sept 2018
Hypovitaminosis D is associated with depression and anxiety in schizophrenia: Results from the national FACE-SZ cohort.
Psychiatry Res. 2018 Sep 13;270:104-110. doi: 10.1016/j.psychres.2018.09.024.
RESULTS: Hypovitaminosis D has been found in 21.4% of the subjects and none of them had received vitamin D supplementation in the previous 12 months. In multivariate analysis, hypovitaminosis D has been significantly associated with respectively higher depressive symptoms (aOR = 1.18 [1.03-1.35], p = 0.02) and current anxiety disorder (aOR = 6.18 [2.15-17.75], p = 0.001), independently of age and gender. No association of hypovitaminosis D with respectively positive and negative symptoms, cognitive scores or other biological variables has been found (all p > 0.05). However, a trend toward significance has been found for metabolic syndrome (p = 0.06).
Vitamin D supplementation has been administered during the previous 12 months in only 8.5% of the subjects but was associated with lower depressive symptoms (aOR = 0.67 [0.46-0.98], p = 0.04) and lower rate of current anxiety disorder (aOR = 0.06 [0.01-0.66], p = 0.02) compared to patients with hypovitaminosis D.
Vitamin D: A potent regulator of dopaminergic neuron differentiation and function - May 2023
📄 Download the PDF from Vitamin D Life
See also web
- Do schizophrenia patients age early? August 2014
- We also propose a role of vitamin D, neuroimmunological changes and elevated oxidative stress as well as mitochondrial dysfunction in addition to the above factors with 'vitamin-D deficiency' as the central paradox
- More than 100 genes linked to schizophrenia identified CBS News July 2014
- Looked at 150,000 people; of which 37,000 had been diagnosed with schizophrenia. (no mention of vitamin D)
- Found 108 genetic markers, 83 of them not previously reported.
- people with the most genetic markers were 15 X more likely to have schizophrenia than those with the fewest markers.
- 📄 Download the PDF from Nature.
- Schizophrenia is 'Orchestra' of Eight Genetically Distinct Disorders with Own Symptoms IBT Sept 2014
- In some patients with hallucinations or delusions, for example, the researchers matched distinct genetic features to patients' symptoms.
- In another group, they found that disorganised speech and behaviour were specifically associated with a set of DNA variations that carried a 100% risk of the illness.
- "When one study would identify an association, no one else could replicate it. What was missing was the idea that these genes don't act independently. They work in concert to disrupt the brain's structure and function, and that results in the illness,"
Vitamin D deficiency and schizophrenia 7 minute video, Dec 2015
schizophrenia Mercola Nov 2016? has the following sections
- Learn More About Schizophrenia; Schizophrenia: Misconception, Facts and Information; What Is Schizophrenia
- Types of Schizophrenia; Schizophrenia in Children; What Causes Schizophrenia?; Is Schizophrenia Hereditary?
- Signs and Symptoms of Schizophrenia; Schizophrenia Diagnosis and Test; Treatment for Schizophrenia
- Famous People with Schizophrenia; Schizophrenia Prevention; Living With Schizophrenia
