Magnesium: intake decreased, difficult to measure in body
Challenges in the Diagnosis of Magnesium Status
Nutrients 2018, 10(9), 1202; https://doi.org/10.3390/nu10091202
by Jayme L. Workinger 1,*,Robert. P. Doyle 2 and Jonathan Bortz 1
1 Human Nutrition and Pharma, Balchem Corporation, 52 Sunrise Park Road, New Hampton, NY 10958, USA
2 Department of Chemistry, Center for Science and Technology, Syracuse University, 111 College Place, Syracuse, NY 13244, USA
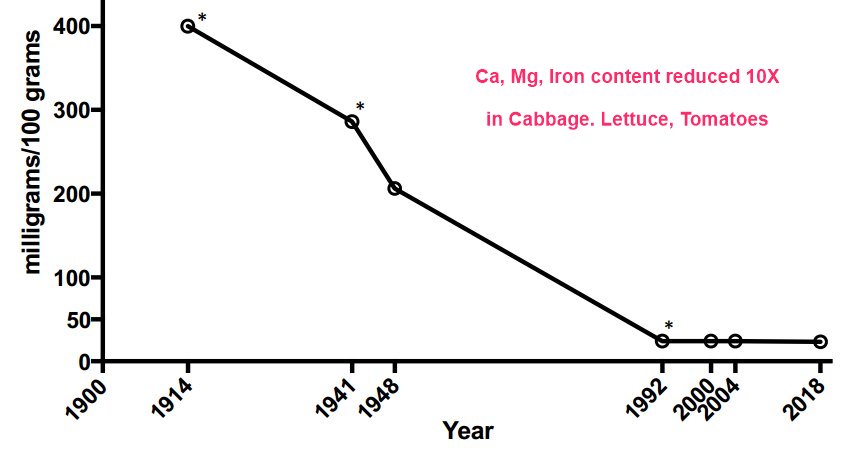
10X Reduction in minerals in some soods
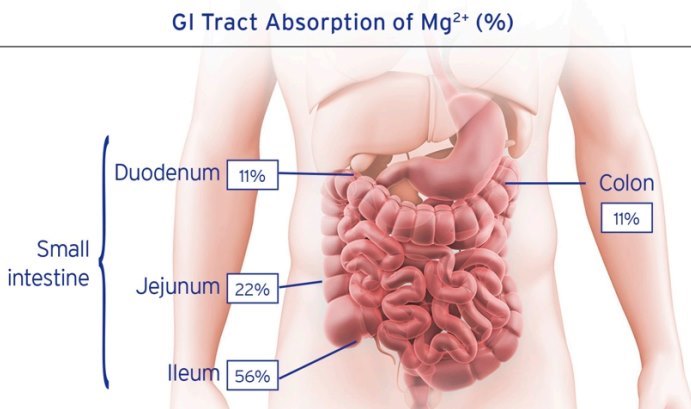
90% of Magnesium absorption is by the small intestine
Magnesium is a critical mineral in the human body and is involved in ~80% of known metabolic functions. It is currently estimated that 60% of adults do not achieve the average dietary intake (ADI) and 45% of Americans are magnesium deficient, a condition associated with disease states like hypertension, diabetes, and neurological disorders, to name a few. Magnesium deficiency can be attributed to common dietary practices, medications, and farming techniques, along with estimates that the mineral content of vegetables has declined by as much as 80–90% in the last 100 years. However, despite this mineral’s importance, it is poorly understood from several standpoints, not the least of which is its unique mechanism of absorption and sensitive compartmental handling in the body, making the determination of magnesium status difficult. The reliance on several popular sample assays has contributed to a great deal of confusion in the literature. This review will discuss causes of magnesium deficiency, absorption, handling, and compartmentalization in the body, highlighting the challenges this creates in determining magnesium status in both clinical and research settings.
📄 Download the PDF from Vitamin D Life
Portions of study
Causes of Magnesium Deficiency
Despite the importance of magnesium to human health and wellness, 60% of people do not meet the recommended DI of 320 mg/day for woman and 420 mg/day for men, with 19% not obtaining even half of the recommended amount [5,6,29]. Magnesium dietary deficiency can be attributed not just to poor mineral intake due to modern diets, but historical farming practices may play a significant role as well. The highest food sources of magnesium are leafy greens (78 mg/serving), nuts (80 mg/serving), and whole grains (46 mg/serving), none of which individually have a high percentage of the recommended dietary allowance (RDA) of magnesium or are eaten consistently or sufficiently for adequate magnesium intake [10,15,30]. Increasing demand for food has caused modern farming techniques to impact the soil’s ability to restore natural minerals such as magnesium. In addition, the use of phosphate-based fertilizers has resulted in the production of aqueously insoluble magnesium phosphate complexes, for example, further depriving the soil of both components [31].
Many fruits and vegetables have lost large amounts of minerals and nutrients in the past 100 years with estimates that vegetables have dropped magnesium levels by 80–90% in the U.S. (Figure 2) and the UK [11,12,13,32,33]. It is important to note that the USDA mineral content of vegetables and fruits has not been updated since 2000, and perhaps even longer, given that the data for 1992 was not able to be definitively confirmed for this review. The veracity of the mineral content to support the claim of demineralization of our food sources should be verified, particularly since farming methods and nutrient fertilization has undoubtedly advanced in the last 50 years. Hence, there is a clear need for a new initiative to study the current mineral content in vegetables and fruits grown in selective markets to get a current and validated assessment of the mineral and nutrient value of commonly consumed fruit and vegetable staples.
Modern dietary practices are now estimated to consist of up to 60% processed foods [38]. Processing techniques, such as grain bleaching and vegetable cooking, can cause a loss of up to 80% of magnesium content [39]. Beverages, such as soft drinks, which contain high phosphoric acid, along with a low protein diet (<30 mg/day), and foods containing phytates, polyphenols and oxalic acid, such as rice and nuts, all contribute to magnesium deficiency due to their ability to bind magnesium to produce insoluble precipitates, thus negatively impacting magnesium availability and absorption [40,41,42,43]. Magnesium in drinking water contributes to about 10% of the ADI [44], however, increased use of softened/purified tap water can contribute to magnesium deficiency due to the filtering or complexation of the metal [45]. In addition, fluoride, found in 74% of the American population’s drinking water, with ~50% of drinking water having a concentration of 0.7 mg/L, prevents magnesium absorption through binding and production of insoluble complexes [46,47,48]. Ingestion of caffeine and alcohol increase renal excretion of magnesium causing an increase in the body’s demand [49,50]. Common medications can also have a deleterious effect on magnesium absorption such as antacids (e.g., omeprazole), due to the increase in gastrointestinal (GI) tract pH (see Section 2.5) [51,52], antibiotics (e.g., ciprofloxacin) [53], and oral contraceptives due to complexation [54,55], and diuretics (e.g., furosemide and bumetanide), due to an increase in renal excretion (see Section 2.6) [56,57].
Factors That Influence Magnesium Absorption
Magnesium concentration within the GI tract is a key driver of how and which of the two transport systems become engaged in magnesium absorption. Active transport in the colon dominates absorption at lower magnesium concentrations but becomes saturated when luminal amounts are between 125 and 250 mg [70,72]. When luminal amounts reach ≥250 mg the absorption mechanism changes and is governed by passive transport in the distal small bowel [70,72].
That being said, the solubility of the magnesium form (inorganic salt, organic salt, chelate, etc.) is an important factor, with increased solubility correlating with increased absorption. The pH of the GI tract can impact how soluble the magnesium form is, with a lower pH increasing magnesium solubility [96,97]. This can make magnesium absorption increasingly difficult as it travels down the small intestine with pH steadily increasing to 7.4 in the ileum. In 2005, Coudray et al. showed that magnesium absorption is significantly affected by GI tract pH in rats [97]. The study showed that as pH gradually increased, the solubility of ten magnesium salts (organic and inorganic) gradually decreased from 85% in the proximal intestine to 50% in the distal intestine. Other studies showed that a commonly used proton pump inhibitor, omeprazole, affected passive transport in vitro [78,79]. They showed that omeprazole suppressed passive magnesium absorption by causing luminal acidity to rise above the range (pH 5.5–6.5) in which claudin 7 and 12 expression is optimized, magnesium hydration shell stripping is most effective, and electrostatic coupling between magnesium and the transporter takes place [79].
Magnesium absorption is enhanced by factors that contribute to water flow across the intestinal mucosal membrane, such as simple sugars and urea [59,98]. Therefore, meals containing carbohydrates and medium chain fatty acids will increase magnesium uptake but will also increase the demand since magnesium is critical to glucose breakdown and insulin release [99]. Solid meals, by prolonging GI transit time, can also enhance magnesium absorption [100]. Increased dietary fiber intake in the diet (e.g., cellulose, pectin, and inulin) does not appear to affect magnesium status but can increase magnesium excretion in feces [101,102,103].
Factors That Affect Magnesium Status
Renal function is a key player in magnesium homeostasis and filters approximately 2400 mg/day [94], and anywhere between 5% and 70% filtered magnesium may actually be excreted in the urine [89,103,104]. This wide range depends on ever changing variables such as dietary intake, existing magnesium status, mobilization from bone and muscle, and the influence of a variety of hormones (e.g., parathyroid hormone, calcitonin, glucagon) [105,106,107] and medications (e.g., diuretics and certain chemotherapies that can cause abnormally high magnesium excretion) [56,90,104,108]. Renal magnesium wasting can occur in patients who are on long-term diuretic management as well as those with diabetes. The resultant magnesium deficiency leads to higher nutritional requirements and the inevitable increase in magnesium absorption to re-establish homeostasis [109].
Gender also contributes to magnesium status as estrogen enhances magnesium utilization, favoring its uptake by soft and hard tissues [110]. Young women have better magnesium retention than young men, and as a result of this, their circulating magnesium levels are lower [111,112], particularly at the time of ovulation or during oral contraceptive use [54,112,113,114,115], when estrogen levels are highest. Consequently, samples taken in a mixed gender population or at time points that do not take this into account could further confound human magnesium studies.
Body mass index (BMI) also may affect magnesium status, particularly in women and children. Patients considered obese (BMI ≥ 30) have been shown to have lower magnesium consumption and reduced magnesium status compared to non-obese age matched controls [116,117,118,119].
Analytical Challenges in Establishing Magnesium Status
Understanding the relationship between the concentration of an analyte in the compartment being measured (e.g., blood, urine, and epithelial samples) and the status of that analyte in the body, or its relevance in the measured compartment is a fundamental principal that will render an analytical test useful or not. Due to the way in which magnesium is compartmentalized, the typical compartment (blood and urine) analytics may not provide an accurate proxy of magnesium status and will mislead the practitioner.
A literature search identified 54 randomized controlled magnesium supplementation studies (see Methods), and showed that the majority of studies examined blood and urine with only a few examining fecal material, other tissues such as muscle, or from different cell specimens (Table 1).
Blood Levels
The current “normal” range interval of serum magnesium is 0.7–1 mmol/L and was established based on serum magnesium levels gathered by a U.S. study between 1971 and 1974 of presumably healthy individuals aged 1–74 years [120]. Serum changes can be influenced by dietary magnesium intake and albumin levels, but can also be affected by short term changes like day to day and hour to hour variability of the amount of magnesium absorbed and excreted through the kidneys [121]. Blood levels have been shown to increase in response to magnesium supplementation, but this does not signal that complete equilibrium has been established between blood and the nearly 100-fold larger body reservoir of magnesium. In fact, the much larger exchangeable pool of magnesium is more often called upon to augment blood levels to maintain a narrow range preferentially, which is a key reason why blood measurements can easily mask deficiency [122,123].
The tight control of magnesium serum levels, representing only 0.8% of total body stores (see Section 2.4), therefore serves as a poor proxy for the 99.2% of magnesium in other tissues that constitutes the body’s true magnesium status. Furthermore, this narrow serum range feeds the common perception of clinicians that magnesium levels rarely fluctuate, and therefore, are not indicative of the condition for which the blood tests are ordered. Therefore, practitioners are apt to order blood tests for magnesium infrequently, if at all, and if a magnesium level is in the patient chart, it is more often as part of a blood test panel and not purposely ordered to determine the magnesium status [89,124,125,126]. This contributes significantly to magnesium deficiency not being recognized as a modifiable nutritional intervention, and magnesium in general, being the neglected mineral that it is.
Red blood cells’ (RBC; erythrocyte and monocyte) magnesium levels are often cited as preferable to serum or plasma levels due to their higher magnesium content (0.5% vs. 0.3%, respectively) . Some RBC studies report correlation to magnesium status particularly when subjects are placed on long-term (~3 months) magnesium replete or deplete diets. However, most studies using RBC magnesium endpoints do not satisfy this long-term design and have not been performed in nearly enough randomized clinical studies to be considered sufficiently robust or reliable (Table 1) [127,128,129]. In addition, the majority of RBC studies do not validate the method through inter-compartmental sampling (e.g., urine and muscle), challenging the claim that this test is a reliable representation of the large magnesium pool.
Urine Levels
Due to the large amount of magnesium filtered and the variable degree of reabsorption and secretion (see Section 2.6), magnesium levels in the urine do not correlate with either the amount of magnesium ingested or the magnesium status in the body . Therefore, despite their frequent use in many published clinical studies (Table 1) [6,130], they should be regarded critically in most clinical and research settings due to the wide fluctuation of renal magnesium reabsorption and excretion.
An epidemiologic study linking magnesium status with risk of heart disease highlighted the poor correlation between urine and blood results and called out the inconsistent results from many previous studies [186,187], even though 24 h urine analyses may still serve some useful function in population based epidemiological studies. The biological variation of magnesium status in smaller cohorts, however, has been highlighted in a study with 60 healthy males in which a within-subject variation of 36% and a between-subject variation of 26% was demonstrated when measuring the 24 h urinary magnesium excretion [187]. The same can be said about fecal magnesium levels, which require 3–7 days collection and are notoriously unpopular with researchers and subjects [69,188].
A more complicated method of determining magnesium status relies on intravenous magnesium loading followed by a 24 h urine collection, ostensibly to measure what percentage of administered dose is retained, from which an assessment of magnesium status can be derived. This retention test relies heavily on the reliability and standardization of the 24 h urine measurement, which is not uniformly accepted [125,189,190,191,192,193]. Additionally, this test is costly, more suitable for research units and impractical for most clinical settings.
Oral Sampling
Energy-dispersive X-ray analysis of magnesium in sublingual cells reports correlation between intracellular magnesium levels in sublingual cells and atrial cell biopsies from subjects undergoing open heart surgery in a small single cohort [194]. However, to our knowledge, this method has not been validated for application as a reliable and indicative of magnesium status in a broader context, beyond a single disease state cohort study. So too, saliva levels have not been adequately correlated with other conventional measurements, and therefore, to date, lack the requisite robustness to be considered as an improvement to assays of blood or urine [155].
Magnesium Isotopes
In recognition of the meaningful exchange of endogenous magnesium between physiologic compartments, and the high degree of biological variability in typical analytic measurements, some researchers maintain that the only reliable way of measuring the disposition of exogenous magnesium is by using isotopic labels [97,195,196,197,198,199,200]. A radioisotope, 28magnesium, has been used previously in magnesium research but it does not make an ideal nucleotide because its half-life (t1/2 = 21 h) [201,202,203] does not match the long biological half-life of magnesium (~1000 h) [201]. Therefore, 28magnesium is not commonly used in current research [128].
Stable isotopes retain all chemical characteristics of an element while being distinguishable from the endogenous elements within the body. This allows for a means of tracking the fate of an exogenously administered “dose” of the element upon ingestion or injection into the body without the harmful emissions associated with radioisotopes. Stable isotopes can be useful tools, particularly in nutritional research, because of the ability to use them in most populations (including small children and pregnant women) and more than one isotope can be used in a study to follow uptake and distribution of different forms of a nutrient.
However, stable magnesium isotopes have proven to be difficult to use because truly low-abundance stable magnesium isotopes do not exist, and therefore, provide significant background noise in the assays. There are three stable magnesium isotopes; 25 magnesium, which has an abundance of 10%, 24magnesium has 79% abundance, and 26 magesnium has 11% abundance. This means that these isotopes cannot be used in the customary small amounts to provide an adequate isotope signal to indicate magnesium status [84]. Very large amounts of isotope, using more than one isotope or significant enrichment, are needed for these studies, dramatically limiting the available supply and adding significantly to the cost, ultimately leading researchers to use less sophisticated and unreliable methods.
Conclusions
An argument can be made for revisiting the accepted ranges of diagnostic tests to capture clinical or other biologic consequences that lie within the currently accepted ranges of normal. Even though this has been suggested in a recent review [6], this approach is likely to be more impactful in large population studies (that have not been undertaken in the U.S. for more than 40 years) than provide pinpoint guidance to diagnose and manage magnesium deficiency in the individual. The multiple factors affecting magnesium status (e.g., dietary intake, luminal concentration, GI pH, weight and gender) in conjunction with the high degree of inter- and intra-variability of intestinal, renal, and tissue handling make an individual diagnosis extremely challenging for the clinician.
Until a commercially viable and unambiguous magnesium deficiency biomarker is identified and validated, it is worth exploring an alternative approach to diagnosing magnesium deficiency. A patient with
dietary risk factors (e.g., high soda, coffee, and processed food ingestion);
using medications known to affect magnesium (e.g., diuretics, antacids, oral contraceptives); with
disease states (e.g., ischemic heart disease, diabetes, and osteoporosis); with
clinical symptoms (e.g., leg cramps, sleep disorder, and chronic fatigue); or with
Metabolic Syndrome (Table 2)
should prompt the practitioner to measure serum and/or 24 h urine for magnesium, bearing in mind that it is quite likely that results from these laboratory tests may read within the reference range (0.75–0.85 mmol/L in the case of serum magnesium) [204].
Vitamin D Life - Magnesium and Vitamin D category contains
{include}
20 most-recently changed items in Magnesium Category
This list is automatically updated
{LISTPAGES}
119 studies cited this study as of June 2022
nothing noticed about new ways to text Magnesium
