Inflammatory bowel diseases are helped by vitamin D – commissioned review
Review article: vitamin D and inflammatory bowel diseases
Alimentary Pharmacology & Therapeutics Article first published online: 17 NOV 2013. DOI: 10.1111/apt.12553
V. P. Mouli 1,
A. N. Ananthakrishnan 2,3,*
1 Department of Gastroenterology, All India Institute of Medical Sciences, New Delhi, India
2 Harvard Medical School, Boston, MA, USA
3 Division of Gastroenterology, Massachusetts General Hospital, Boston, MA, USA
Correspondence to: Dr A. N. Ananthakrishnan, Crohn's & Colitis Centre, Massachusetts General Hospital, 165 Cambridge Street, 9th Floor, Boston, MA 02114, USA. [email protected]
This commissioned review article was subject to full peer review and the authors received an honorarium from Wiley on behalf of AP&T.;
Background: Vitamin D is traditionally associated with bone metabolism.
The immunological effects of vitamin D have increasingly come into focus.
Aims: To review the evidence supporting a role of vitamin D in inflammatory bowel diseases.
Methods: A comprehensive search was performed on PubMed using the terms ‘crohn's disease’ ‘ulcerative colitis’ and ‘vitamin D’.
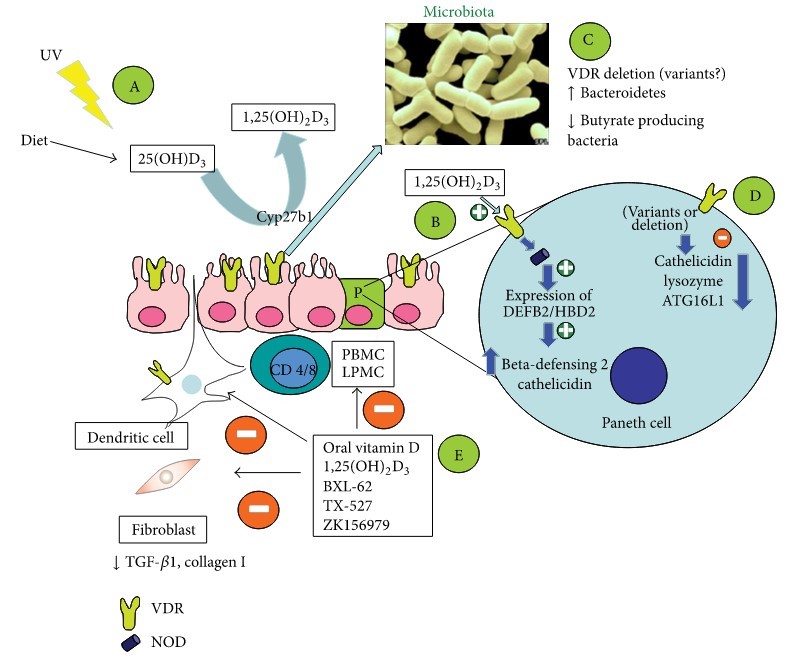
Results: Vitamin D deficiency is common in patients with inflammatory bowel diseases (IBD) (16–95%) including those with recently diagnosed disease. Evidence supports immunological role of vitamin D in IBD. In animal models, deficiency of vitamin D increases susceptibility to dextran sodium sulphate colitis, while 1,25(OH)2D3 ameliorates such colitis. One prospective cohort study found low predicted vitamin D levels to be associated with an increased risk of Crohn's disease (CD). Limited data also suggest an association between low vitamin D levels and increased disease activity, particularly in CD. In a large cohort, vitamin D deficiency (<20 ng/mL) was associated with increased risk of surgery (OR 1.8, 95% CI 1.2–2.5) in CD and hospitalisations in both CD (OR 2.1, 95% CI 1.6–2.7) and UC (OR 2.3, 95% CI 1.7–3.1). A single randomised controlled trial demonstrated that vitamin D supplementation may be associated with reduced frequency of relapses in patients with CD compared with placebo (13% vs. 29%, P = 0.06).
Conclusions: There is growing epidemiological evidence to suggest a role for vitamin D deficiency in the development of IBD and also its influence on disease severity. The possible therapeutic role of vitamin D in patients with IBD merits continued investigation.
Clipped from PDF
Studies
Intervention: Crohn's and Ulcerative colitis
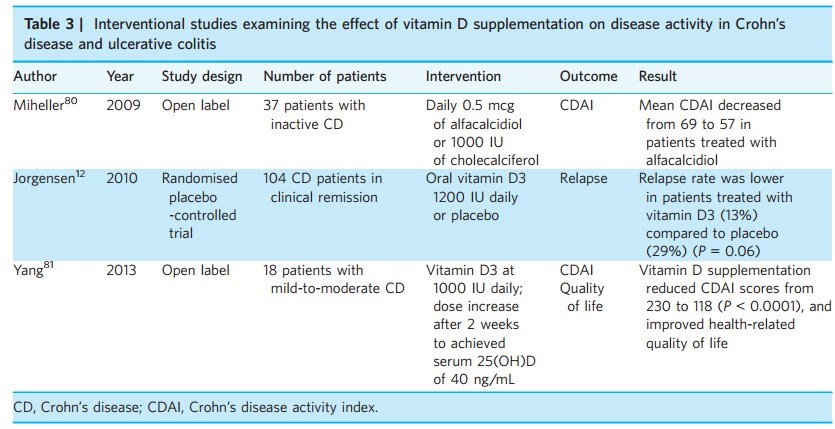
Table 4 | Unanswered clinical questions regarding the role of vitamin D in inflammatory bowel diseases
Does low serum vitamin D cause Crohn's disease or ulcerative colitis, or is it a marker for other risk factors?
. Can supplementation with vitamin D in high-risk individuals prevent or delay the onset of Crohn's disease or ulcerative colitis?
Does vitamin D deficiency cause a more severe phenotype or increased inflammatory activity in Crohn's disease,
- or is it merely a consequence of severity of disease?
- Is vitamin D status predictive of recurrence of Crohn's disease post-operatively?
- What is the optimal role of vitamin D supplementation as a therapeutic modality in patients with IBD?
- Induction of remission?
- Maintenance of remission and prevention of relapse?
- Prevention of post-operative recurrence?
What is the optimal serum 25(OH)D level for its effect on inflammation in patients with IBD?
What is the optimal dose and modality for treatment of vitamin D deficiency in IBD patients?
Can vitamin D supplementation reduce risk of colorectal cancer in IBD?
PDF is attached at the bottom of this page
See also Vitamin D Life
Inflammatory bowel diseases treated with vitamin D – Review May 2014
Inflammatory bowel disease and vitamin D – review Aug 2012 previous article in same journal
Irritable Bowel Syndrome: social media indicates that vitamin D is a good treatment – Oct 2013
70 percent of people with IBS had symptoms relieved with high dose vitamin D – 2012
IBD in Finland – 3X increase in 15 years, more prevalent further from equator – Nov 2012
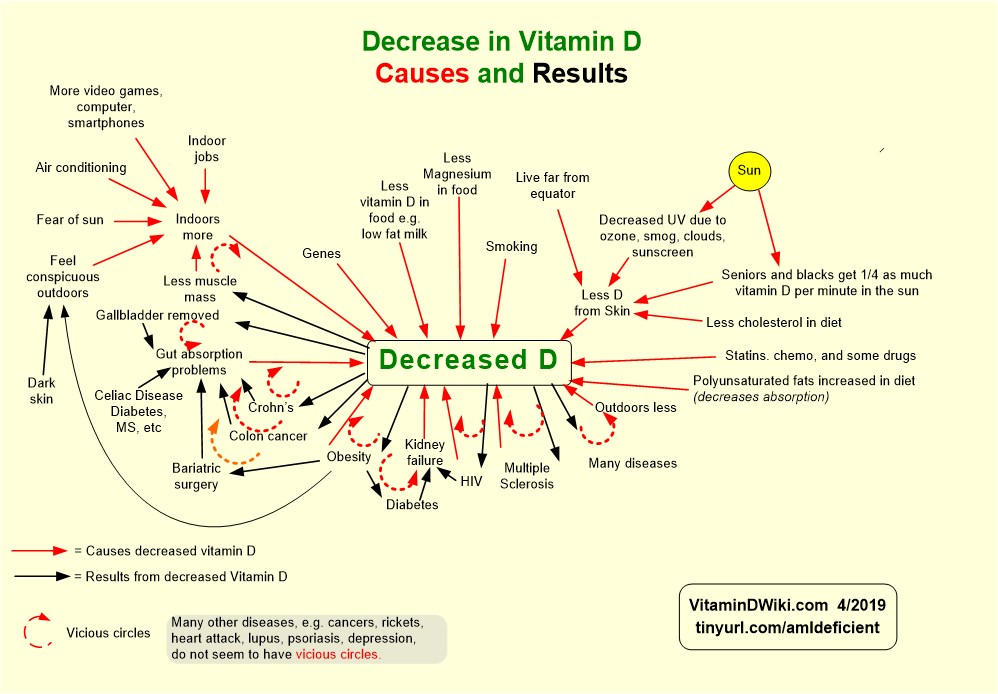
Overview Gut and vitamin D contains the following summary and chart (see lower left)
- {include}