Inflammatory bowel disease – Vitamin D looks promising
Vitamin D as a novel therapy in inflammatory bowel disease: new hope or false dawn?
O'Sullivan M1.
Proc Nutr Soc. 2015 Feb;74(1):5-12. doi: 10.1017/S0029665114001621. Epub 2014 Dec 10.
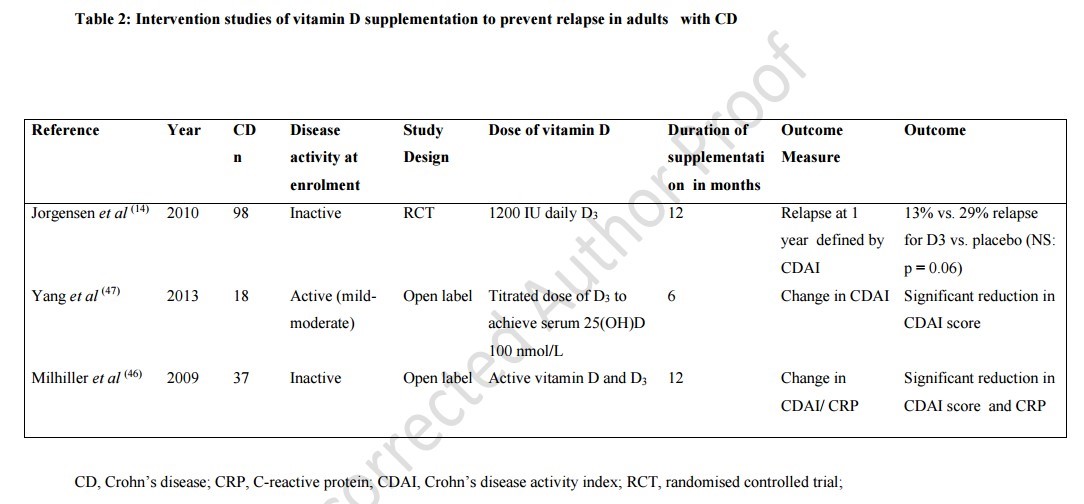
There is increasing scientific interest in the field of vitamin D research, moving the focus beyond bone health to other disease processes. Low circulating vitamin D levels have been reported as a risk factor for several pathophysiologically divergent diseases, including cancers, diabetes, CVD, multiple sclerosis and inflammatory diseases, including rheumatoid arthritis and inflammatory bowel disease (IBD). But, therein, remains the challenge: can any single nutrient contribute to multiple complex disease mechanisms and, ultimately, have therapeutic potential? The aim of this review is to critically evaluate several strands of scientific evidence surrounding vitamin D and inflammation, primarily focusing on IBD. Epidemiological studies suggest an increased incidence of IBD and rheumatoid arthritis in countries of more northern latitudes, mirroring sunlight patterns. A considerable body of evidence supports the anti-inflammatory effects of vitamin D, at least in animal models of IBD. Although it is accepted that suboptimal vitamin D status is common in IBD, some studies suggest that this associates with more severe disease. With regard to treatment, the data are only beginning to emerge from randomised controlled trials to suggest that people with IBD may remain in remission longer when treated with oral vitamin D. In conclusion, several strands of evidence suggest that vitamin D may modify the immune response in IBD. There is a continued need for large well-designed clinical trials and mechanistic studies to determine if, and how, this emerging promise translates into tangible clinical benefits for people with chronic debilitating diseases such as IBD.
PMID: 25490986