HPV and Vitamin D - several studies
HPV warts treated by both Intralesional and topical Vitamin D - March 2024
Vitamin D and HPV infection: Clinical pearls
J Cosmet Dermatol. 2024 Mar 15. doi: 10.1111/jocd.16280
Zeinab Aryanian 1 2 3, Kamran Balighi 1 3, Azadeh Goodarzi 4 5, Zeinab Mohseni Afshar 6, Parvaneh Hatami 1
📄 Download the PDF from Vitamin D Life
31 References
Priya A, Adil M, Suhail Amin S, Mohtashim M, Bansal R, Alam M. Intralesional vitamin D3 in recalcitrant palmoplantar and periungual warts : a prospective, observational study. Acta Dermatovenerol Croat. 2019;27(4):215.
Kazeminejad A, Ghahari MJ, Hajheydari Z. Treatment of warts in children with focus on recalcitrant warts : a narrative review. J Pediatr Rev. 2020;8(4):237-246.
Liu PT, Stenger S, Li H, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006;311(5768):1770-1773.
Kavya M, Shashikumar BM, Harish MR, Shweta BP. Safety and efficacy of intralesional vitamin D3 in cutaneous warts : an open uncontrolled trial. J Cutan Aesthet Surg. 2017;10(2):90-94.
Bouillon R. Extra-skeletal effects of vitamin D. Front Horm Res. 2018;50:72-88.
Fathy G, Sharara MA, Khafagy AH. Intralesional vitamin D3 versus Candida antigen immunotherapy in the treatment of multiple recalcitrant plantar warts : a comparative case-control study. Dermatol Ther. 2019;32(5):e12997.
Raghukumar S, Ravikumar B, Vinay K, Suresh M, Aggarwal A, Yashovardhana D. Intralesional vitamin D3 injection in the treatment of recalcitrant warts : a novel proposition. J Cutan Med Surg. 2017;21(4):320-324.
Tamer F, Eren Yuksel M, Karabag Y. Pre-treatment vitamin B12, folate, ferritin, and vitamin D serum levels in patients with warts : a retrospective study. Croat Med J. 2020;61(1):28-32.
Shalaby ME, Hasan MS, Elshorbagy MS, Abo Raya AR, Elsaie ML. Diagnostic and therapeutic implications of vitamin D deficiency in patients with warts : a case-controlled study. J Cosmet Dermatol. 2022 Mar;21(3):1135-1142. doi:10.1111/jocd.14156
Tawfik N, Hussein HI, Hassan RM, Atwa MA. Assessment of serum 25-hydroxycholecalciferol level in patients with recalcitrant palmoplantar warts . Suez Canal Univ Med J. 2020;23(2):129-134.
Imagawa I, Suzuki H. Successful treatment of refractory warts with topical vitamin D3 derivative (maxacalcitol, 1α, 25-dihydroxy-22-oxacalcitriol) in 17 patients. J Dermatol. 2007;34(4):264-266.
Moscarelli L, Annunziata F, Mjeshtri A, et al. Successful treatment of refractory wart with a topical activated vitamin D in a renal transplant recipient. Case Rep Transplant. 2011;2011:368623.
Al-Sabak H, Al-Hattab M, Al-Rammahi M, Al-Dhalimi M. The efficacy of intralesional vitamin D3 injection in the treatment of cutaneous warts : a clinical therapeutic trial study. Skin Res Technol. 2023 Aug;29(8):e13442. doi:10.1111/srt.13442
Aktas H, Ergin C, Demir B, Ekiz O. Intralesional vitamin D injection may be an effective treatment option for warts . J Cutan Med Surg. 2016;20:118-122.
Naresh M. A study of effectiveness of intralesional vitamin D3 in treatment of multiple cutaneous warts . IOSR J Dent Med Sci. 2019;18(3):84-87.
El Sayed MH, Sayed FS, Afify AA. Intralesional zinc sulphate 2% versus intralesional vitamin D in plantar warts : a clinicodermoscopic study. Dermatol Ther. 2020;33(3):e13308.
Mohamed EEM, El Taieb MA, Abd El-Sabour GA. Intralesional vitamin D3 versus purified protein derivatives in the treatment of multiple cutaneous warts : comparative study. Egypt J Hosp Med. 2019;76(2):3589-3594.
Shaldoum DR, Hassan GFR, El Maadawy EH, El-Maghraby GM. Comparative clinical study of the efficacy of intralesional MMR vaccine vs intralesional vitamin D injection in treatment of warts . J Cosmet Dermatol. 2020;19:2033-2040.
Raveendra L, Raju BP, Dharam KK, Yadav VMK. Comparison of purified protein derivative and vitamin D in the treatment of recalcitrant warts . Clin Dermatol Rev. 2021;5(1):54.
Yousaf F, Raza N, Ahmed N, Sadiq S, Anwar A. Comparison of intralesional Vitamin D3 versus cryotherapy for management of plantar warts . PAFMJ. 2019;69(6):1304-1308.
Tawfik YM, Hosny AH, El-Gazzar AF, Bakr RM. Efficacy and safety of treating anogenital warts with intralesional vitamin D3 injection: a report on 20 Egyptian patients. Al-Azhar Assiut Med J. 2020;18(2):140.
Milante RR, Venida-Tablizo A, King-Ismael D. Efficacy and safety of single versus multiple intralesional immunotherapy with purified protein derivative (PPD) in the treatment of multiple verruca vulgaris. Int J Dermatol. 2019;58(12):1477-1482.
Ezquerra GM, Regaña MS, Millet PU. Combination of acitretin and oral calcitriol for treatment of plaque-type psoriasis. Acta Derm Venereol. 2007;87(5):449-450.
Singh M, Thakral D, Kar HK, Rishi N, Sharma PK, Mitra DK. Distinct clinico-immunological profile of patients infected with human papilloma virus genotypes 6 and 11. VirusDisease. 2017;28(2):200-204.
Abdel-Azim ES, Abdel-Aziz RT, Ragaie MH, Mohamed EA. Clinical and dermoscopic evaluation of intralesional vitamin D3 in treatment of cutaneous warts : a placebo-controlled study. J Egypt Women's Dermatol Soc. 2020;17(1):6.
El-Taweel AEA, Salem RM, Allam AH. Cigarette smoking reduces the efficacy of intralesional vitamin D in the treatment of warts . Dermatol Ther. 2019;32(2):e12816.
Attwa E, Elawady R, Salah E. ‘Cryo-immuno-therapy’ is superior to intralesional Candida antigen monotherapy in the treatment of multiple common warts . J Dermatol Treat. 2021;32(8):1018-1025.
Yeh MC-H, Tsai T-Y, Huang Y-C. Intralesional vitamin D3 injection in the treatment of warts : a systematic review and meta-analysis. J Am Acad Dermatol. 2020;82(4):1013-1015.
Kareem IMA, Ibrahim IM, Mohammed SF, Ahmed AAB. Effectiveness of intralesional vitamin D3 injection in the treatment of common warts : single-blinded placebo-controlled study. Dermatol Ther. 2019;32(3):e12882.
Note: Both methods provide a much higher concentration of wart Vitamin D than from oral Vitamin D
Vitamin D Life – Injection contains:
{include}
Vitamin D Life – Topical Vitamin D category contains:
{include}
Vitamin D Life – Warts removed by vitamin D injection - many studies
HPV and Vitamin D association - no consensus - Review Jan 2024
Relationship between human papillomavirus and serum vitamin D levels: a systematic review
BMC Infect Dis. 2024 Jan 13;24(1):80. doi: 10.1186/s12879-024-09006-8.
Seyedeh Maryam Khalili 1, Elnaz Haji Rafiei 1, Marjan Havaei 1, Leila Alizadeh 1, Fereshte Ghahremani 1, Zohreh Keshavarz 2, Ali Montazeri 3 4, Hedyeh Riazi 5
Background: Human papillomavirus (HPV) is one of the most prevalent sexually transmitted diseases worldwide. The present review was conducted to accumulate evidence on the relationship between cervicovaginal human papillomavirus infection and serum vitamin D status.
Methods: Electronic databases including Web of Science, Embase, Scopus, and PubMed were searched by different combinations of keywords related to "human papillomavirus" and "vitamin D", obtained from Mesh and Emtree with AND, and OR operators without any time restriction until December 24, 2022. Selection of articles was based on the inclusion and exclusion criteria. Newcastle-Ottawa Scale was used for quality assessment. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist was applied for reporting.
Results: In total, 276 citations were retrieved. After removing duplicates, and non-related articles, the full texts of 7 articles were reviewed including 11168 participants.
Three studies reported that there was a positive relationship between vitamin D deficiency and cervicovaginal human papillomavirus while
Three studies did not.
One study showed a significant positive association between higher vitamin D stores and short-term high-risk human papillomavirus persistence.
Conclusions: The findings showed no firm evidence for any association between serum vitamin D level and cervicovaginal human papillomavirus infection, although the possible association could not be discarded. Further investigations are needed to reach sound evidence.
📄 Download the PDF from Vitamin D Life
44 References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492 . - DOI - PubMed
Rosales R, Rosales C. Immune therapy for human papillomaviruses-related cancers. World J Clin Oncol. 2014;5(5):1002–19. https://doi.org/10.5306/wjco.v5.i5.1002 . - DOI - PubMed - PMC
Okunade KS. Human papillomavirus and cervical cancer. J Obstet Gynaecol. 2020;40(5):602–8. https://doi.org/10.1080/01443615.2019.1634030 . - DOI - PubMed
Seong J, Ryou S, Lee J, Yoo M, Hur S, Choi B-S. Enhanced disease progression due to persistent HPV -16/58 infections in Korean women: a systematic review and the Korea HPV cohort study. Virol J. 2021;18(1):1–13. https://doi.org/10.1186/s12985-021-01657-2 . - DOI
Choi S, Ismail A, Pappas-Gogos G, Boussios S. HPV and cervical cancer: A review of epidemiology and screening uptake in the UK. Pathogens. 2023;12(2):298. https://doi.org/10.3390/pathogens12020298 . - DOI - PubMed - PMC
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660 . - DOI - PubMed
Stelzle D, Tanaka LF, Lee KK, et al. Estimates of the global burden of cervical cancer associated with HIV. Lancet Glob Health 2020; published online Nov 16. S2214-109X(20)30459-9
Momenimovahed Z, Mazidimoradi A, Maroofi P, Allahqoli L, Salehiniya H, Alkatout I. Global, regional and national burden, incidence, and mortality of cervical cancer. Cancer Rep. 2023;6(3):e1756. https://doi.org/10.1002/cnr2.1756 . - DOI
Kombe Kombe AJ, Li B, Zahid A, Mengist HM, Bounda GA, Zhou Y, Jin T. Epidemiology and burden of human papillomavirus and related diseases, molecular pathogenesis, and vaccine evaluation. Front Public Health. 2021;20(8):552028. https://doi.org/10.3389/fpubh.2020.552028 . - DOI
Ono A, Koshiyama M, Nakagawa M, Watanabe Y, Ikuta E, Seki K, Oowaki M. The preventive effect of dietary antioxidants on cervical cancer development. Medicina (Kaunas). 2020;56(11):604. https://doi.org/10.3390/medicina56110604 . - DOI - PubMed
Lopes RDVC, Teixeira JA, Marchioni D, Villa LL, Giuliano AR, Luiza Baggio M, Fisberg RM. Dietary intake of selected nutrients and persistence of HPV infection in men. Int J Cancer. 2017;141(4):757–65. https://doi.org/10.1002/ijc.30772 . - DOI - PubMed - PMC
Albergamo A, Apprato G, Silvagno F. The role of vitamin D in supporting health in the COVID-19 Era. Int J Mol Sci. 2022;23(7):3621. https://doi.org/10.3390/ijms23073621 . - DOI - PubMed - PMC
Colotta F, Jansson B, Bonelli F. Modulation of inflammatory and immune responses by vitamin D. J Autoimmun. 2017;85:78–97. https://doi.org/10.1016/j.jaut.2017.07.007 . - DOI - PubMed
Di Rosa M, Malaguarnera M, Nicoletti F, Malaguarnera L. Vitamin D3: a helpful immuno-modulator. Immunology. 2011;134(2):123–39. https://doi.org/10.1111/j.1365-2567.2011.03482.x . - DOI - PubMed - PMC
Weir EK, Thenappan T, Bhargava M, Chen Y. Does vitamin D deficiency increase the severity of COVID-19? Clin Med (Lond). 2020;20(4):e107–8. https://doi.org/10.7861/clinmed.2020-0301 . - DOI - PubMed
Wang H, Chen W, Li D, Yin X, Zhang X, Olsen N, Zheng SG. Vitamin D and chronic diseases. Aging Dis. 2017; 8(3):346-353. https://doi.org/10.14336/AD.2016.1021 . PMID: 28580189.
Teymoori-Rad M, Shokri F, Salimi V, Marashi SM. The interplay between vitamin D and viral infections. Rev Med Virol. 2019;29(2):e2032. https://doi.org/10.1002/rmv.2032 . - DOI - PubMed
Wei R, Christakos S. Mechanisms underlying the regulation of innate and adaptive immunity by vitamin D. Nutrients. 2015;7(10):8251–60. https://doi.org/10.3390/nu7105392 . - DOI - PubMed - PMC
Yamshchikov AV, Desai NS, Blumberg HM, Ziegler TR, Tangpricha V. Vitamin D for treatment and prevention of infectious diseases: a systematic review of randomized controlled trials. Endocr Pract. 2009;15(5):438–49. https://doi.org/10.4158/EP09101.ORR . - DOI - PubMed - PMC
Shim J, Pérez A, Symanski E, Nyitray AG. Association between serum 25-hydroxyvitamin D level and human papillomavirus cervicovaginal infection in women in the United States. J Infect Dis. 2016;213(12):1886–92. https://doi.org/10.1093/infdis/jiw065 . - DOI - PubMed
Özgü E, Yılmaz N, Başer E, Güngör T, Erkaya S, Yakut Hİ. Could 25-OH vitamin D deficiency be a reason for HPV infection persistence in cervical premalignant lesions? J Exp Ther Oncol. 2016;11(3):177–80 (PMID: 28471122). - PubMed
El Mongy NN, Hilal RF, Badr AM, Alraawi SA. Serum vitamin D level in patients with viral warts. J Egypt Women’s Dermatologic Soc. 2018;15(3):133–8. - DOI
García-Carrasco M, Mendoza-Pinto C, Munguía-Realpozo P, et al. Lack of association between serum 25-hydroxyvitamin D levels and cervical human papillomavirus infection in systemic lupus erythematosus. Lupus. 2015;24(6):606–12. https://doi.org/10.1177/0961203314559628 . - DOI - PubMed
El-Zein M, Khosrow-Khavar F, Burchell AN, Tellier PP, Eintracht S, McNamara E, Coutlée F, Franco EL; HITCH study group. Association of serum 25-hydroxyvitamin D with prevalence, incidence, and clearance of vaginal HPV infection in young women. J Infect Dis. 2021; 224(3):492-502. https://doi.org/10.1093/infdis/jiaa758 .
Page M J, McKenzie J E, Bossuyt P M, Boutron I, Hoffmann T C, Mulrow C D et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews BMJ 2021; 372 :n71. https://doi.org/10.1136/bmj.n71 .
Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;1(14):45. https://doi.org/10.1186/1471-2288-14-45 . - DOI
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available from: URL: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm .
Chu TW, Jhao JY, Lin TJ, Lin TW, Wang CL, Chang HS, Liu LC, Chang CC. Vitamin D in gynecological diseases. J Chin Med Assoc. 2021;84(11):1054–9. https://doi.org/10.1097/JCMA.0000000000000607 . - DOI - PubMed
Troja C, Hoofnagle AN, Szpiro A, Stern JE, Lin J, Winer RL. Understanding the role of emerging Vitamin D biomarkers on short-term persistence of high-risk human papillomavirus infection among mid-adult women. J Infect Dis. 2021;224(1):123–32. https://doi.org/10.1093/infdis/jiaa711 . - DOI - PubMed
Troja C, Hoofnagle AN, Szpiro A, Stern JE, Lin J, Winer RL. Serum concentrations of emerging vitamin D biomarkers and detection of prevalent high-risk HPV infection in mid-adult women. Cancer Epidemiol Biomarkers Prev. 2020;29(7):1468–74. https://doi.org/10.1158/1055-9965.EPI-20-0126 . - DOI - PubMed - PMC
Mertoğlu C, Naykı Ü, Naykı C, Günay M. The relationship between vitamin D And human papilloma virus infection. J Clin Anal Med. 2017;8(6):538–40. https://doi.org/10.4328/JCAM.5400 . - DOI
Çakir AT, Özten MA. Serum vitamin D levels in high-risk HPV infected patients, is there any relation? J Clin Med Kaz. 2022; 19(3):35-39. https://doi.org/10.23950/jcmk/12113 .
Siddiqui M, Manansala JS, Abdulrahman HA, Nasrallah GK, Smatti MK, Younes N, Althani AA, Yassine HM. Immune modulatory effects of vitamin D on viral infections. Nutrients. 2020;12(9):2879. https://doi.org/10.3390/nu12092879 . - DOI - PubMed - PMC
Beard JA, Bearden A, Striker R. Vitamin D and the anti-viral state. J Investig Med. 2011;50(3):194–200.
Gallo D, Baci D, Kustrimovic N, Lanzo N, Patera B, Tanda ML, Piantanida E, Mortara L. How does vitamin D affect immune cells crosstalk in autoimmune diseases? Int J Mol Sci. 2023;24(5):4689. https://doi.org/10.3390/ijms24054689 . - DOI - PubMed - PMC
Sun J, Zhang YG. Vitamin D receptor influences intestinal barriers in health and disease. Cells. 2022;11(7):1129. https://doi.org/10.3390/cells11071129 . - DOI - PubMed - PMC
Hewavisenti RV, Arena J, Ahlenstiel CL, Sasson SC. Human papillomavirus in the setting of immunodeficiency: Pathogenesis and the emergence of next-generation therapies to reduce the high associated cancer risk. Front Immunol. 2023;14:1112513. https://doi.org/10.3389/fimmu.2023.1112513 . - DOI - PubMed - PMC
Piotrowska A, Wierzbicka J, Żmijewski MA. Vitamin D in the skin physiology and pathology. Acta Biochim Pol. 2016;63(1):17–29. https://doi.org/10.18388/abp.2015_1104 . - DOI - PubMed
Fleet JC, DeSmet M, Johnson R, Li Y. Vitamin D and Cancer: A review of molecular mechanisms. Biochem J. 2011;441(1):61. https://doi.org/10.1042/BJ20110744 . - DOI
Gunville CF, Mourani PM, Ginde AA. The role of vitamin D in prevention and treatment of infection. Inflamm Allergy Drug Targets. 2013;12(4):239. https://doi.org/10.2174/18715281113129990046 . - DOI - PubMed - PMC
Fathi N, Ahmadian E, Shahi S, Roshangar L, Khan H, Kouhsoltani M, Maleki Dizaj S, Sharifi S. Role of vitamin D and vitamin D receptor (VDR) in oral cancer. Biomed Pharmacother. 2019;109:391–401. https://doi.org/10.1016/j.biopha.2018.10.102 . - DOI - PubMed
Avila E, Noriega-Mejía BJ, González-Macías J, Cortes-Hernández U, García-Quiroz J, García-Becerra R, Díaz L. The preventive role of the vitamin D endocrine system in cervical cancer. Int J Mol Sci. 2023;24(10):8665. https://doi.org/10.3390/ijms24108665 . - DOI - PubMed - PMC
Zhu G, Li Z, Tang L, Shen M, Zhou Z, Wei Y, Zhao Y, Bai S, Song L. Associations of dietary intakes with gynecological cancers: Findings from a cross-sectional study. Nutrients. 2022;14(23):5026. https://doi.org/10.3390/nu14235026 . - DOI - PubMed - PMC
Koc S, Kurt S, Ilgen O, Timur H, Uslu T. The effect of vitamin D on the regression of human papilloma virus infection and metabolic parameters: a retrospective study. Eur J Gynaecol Oncol. 2021;42(2):340–5. https://doi.org/10.31083/j.ejgo.2021.02.2246) . - DOI
300,000 IU monthly oral Vitamin D got levels to only 24 ng, no HPV benefit - 2021
The effect of vitamin D on the regression of human papilloma virus infection and metabolic parameters: a retrospective study
EUROPEAN J. OF GYNAECOLOGICAL ONCOLOGY, vol.42, no.2, pp.340-345, 2021 10.31083/j.ejgo.2021.02.2246
Koc S., KURT S., İLGEN O., Timur H. T., Uslu T.
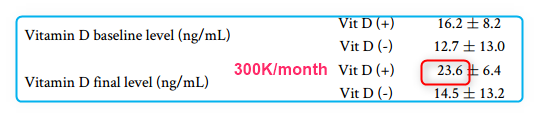
Purpose: Human papillomavirus (HPV) is the primary cause of cervical cancer. Our study aims to evaluate the effects of vitamin D on HPV regression, related cytological pathologies and various metabolic parameters.
Materials and methods: 100 high-risk HPV positive patients, who were detected from hospital database, were divided into 2 groups as those who received vitamin D supplements (n = 50) and did not receive vitamin D supplements (n = 50). We determined the changes in serum vitamin D concentrations, metabolic parameters of patients and regression of HPV after 6 months. Then, we compared the results of patients who took vitamin D supplements, and those who did not.
Results: Patient characteristics of both groups were similar in terms of smoking, using oral contraceptives, operation status, body mass index, and mean age of first coitus. Considering the findings of our study, the difference in rate of HPV regression was not significant in the group with a history of vitamin D use (P = 0.804). Regarding metabolic parameters, we observed significant decrease in insulin (P < 0.001), triglyceride (P = 0.019), and CRP (P < 0.001) levels in the group with a history of vitamin D use.
Conclusion: According to our findings, vitamin D supplementation does not significantly increase the rate of HPV regression. On the other hand, its metabolic effects are noteworthy. It has positive effects on glucose homeostasis and lipid profile. In the light of previous studies, vitamin D may be helpful in the treatment of vaginal infections, nonetheless it is not a as effective concerning cervical HPV infections.
📄 Download the PDF from Vitamin D Life
HPV 1.8X more likely if low Vitamin D - Nov 2020
Understanding the role of emerging vitamin D biomarkers on short-term persistence of high-risk HPV infection among mid-adult women - Nov 2020
J Infect Dis,. 2020 Nov 17;jiaa711. doi: 10.1093/infdis/jiaa711
Catherine Troja 1, Andrew N Hoofnagle 2, Adam Szpiro 3, Joshua E Stern 4, John Lin 1, Rachel L Winer 1
Background: Associations between vitamin D biomarkers and persistent high-risk human papillomavirus (hrHPV) detection have not been evaluated.
Methods: 2011-2012 stored sera from 72 women ages 30-50 years with prevalent hrHPV (n=116 type-specific infections) were tested for 5 vitamin D biomarkers: 25(OH)D and 4 emerging biomarkers, 1,25(OH)2D, 24,25(OH)2D, free vitamin D, and vitamin D binding protein (DBP). hrHPV detection patterns (persistent versus transient/sporadic) were determined using cervicovaginal swabs collected monthly for 6 months. Associations between vitamin D and short-term type-specific hrHPV persistence were estimated using logistic regression. Our primary exposure was continuous 25(OH)D, with additional biomarkers evaluated as secondary exposures. Primary models adjusted for age, race, BMI, education, contraceptives, smoking, season, and calcium/phosphate levels. Sensitivity analyses restricted from 19 hrHPV types to 14 used in cervical cancer screening.
Results: In primary analyses, non-significant positive associations with hrHPV persistence were observed for measures of 25(OH)D and 24,25(OH)2D. Associations were stronger and significant restricting to 14 hrHPV types (25(OH)D per 10ng/mL increase:
aOR=1.82,95%CI:1.15-2.88 and
aOR=4.19,95%CI:1.18-14.88 DBP-adjusted;
25(OH)D≥30 vs <30ng/mL: aOR=8.85,95%CI:2.69-29.06;
24,25(OH)2D: aOR=1.85,95%CI:1.18-2.88).
1,25(OH)2D was unassociated with persistence.
Conclusions: Serum vitamin D measured by multiple biomarkers showed positive associations with short-term hrHPV persistence that were significant only when restricting to 14 clinically-relevant hrHPV types.
HPV 3X more likely if low Vitamin D - 2016
Association Between Serum 25-Hydroxyvitamin D Level and Human Papillomavirus Cervicovaginal Infection in Women in the United States.
J Infect Dis. 2016 Jun 15;213(12):1886-92. doi: 10.1093/infdis/jiw065
Shim J1, Pérez A2, Symanski E3, Nyitray AG3.
1 Department of Business Intelligence and Analytics, Texas Children's Health Plan, Houston.
2 Department of Biostatistics, University of Texas School of Public Health, Austin.
3 Department of Epidemiology, Human Genetics, and Environmental Sciences, University of Texas School of Public Health, Houston.
📄 Download the PDF from Vitamin D Life
BACKGROUND:
A sufficient level of vitamin D enhances protection against several infectious diseases; however, its association with cervicovaginal human papillomavirus (HPV) infection has not been studied.
METHODS:
Data for this cross-sectional study were from National Health and Nutrition Examination Survey 2003-2006. A total of 2353 sexually active women for whom cervicovaginal HPV infection status and serum 25-hydroxyvitamin D (25[OH]D) level were known were studied. Associations between serum 25(OH)D levels (continuous and categorical forms) and cervicovaginal HPV infection (due to high-risk HPV or vaccine-type HPV) were estimated using weighted logistic regression.
RESULTS:
After adjustment for age, race/ethnicity, and marital status, the odds of high-risk HPV infection were increased per each 10 ng/mL decrease in serum 25(OH)D level (adjusted odds ratio [aOR], 1.14; 95% confidence interval [CI], 1.02-1.27). Similarly, the odds of vaccine-type HPV infection were increased in women with vitamin D levels that were severely deficient (serum 25[OH]D level, <12 ng/mL; aOR, 2.90 ; 95% CI, 1.32-6.38), deficient (12-19 ng/mL; aOR, 2.19; 95% CI, 1.08-4.45), and insufficient (20-29 ng/mL; aOR, 2.19; 95% CI, 1.22-3.93), compared with those with vitamin D levels that were sufficient (≥30 ng/mL).
CONCLUSIONS:
Cervicovaginal HPV prevalence is associated with less-than-optimal levels of serum vitamin D.
See also web
40 HPV strains cause Cancer Mercola Dec 2022
cervical, penile, oral, vaginal, vulvar and anal cancer.
"Ninety percent of HPV infections resolve on their own without treatment, as a well-functioning immune system will keep the virus in check. In rare cases, however, infection with a high-risk HPV that remains untreated and unchecked may turn into cancer."
"In the U.S., 3% of all cancers in women and 2% of cancers in men are related to untreated chronic HPV infection.2"
7 Million American Men Carry Cancer-Causing HPV NYT Oct 2017
- "The study, in the Annals of Internal Medicine, found that 11 million men and 3.2 million women in the United States had oral HPV infections. Among them, 7 million men and 1.4 million women had strains that can cause cancers of the throat, tongue and other areas of the head and neck."
- “The difference in oral HPV infection between smokers and nonsmokers is staggering,” Note by Vitamin D Life: Smoking reduces vitamin D - many studies
- Natural Herbal HPV "Cure" Discovered GreeMedInfo Jan 2018
- curcumin (which activates the vitamin D receptor), reetha, amla and aloe vera vaginal cream
ChatGPT description of HPV Jan 2024
HPV stands for Human Papillomavirus, a group of more than 200 related viruses. Some types of HPV are considered high-risk because they can cause cancer, including cervical cancer in women, as well as other types of cancer in both men and women. Other types of HPV can cause warts on different parts of the body, including genital warts.
Most HPV infections don't lead to cancer and go away on their own within two years. However, the infection can persist and cause long-term problems. Vaccines are available that can protect against the most dangerous types of HPV and are typically recommended for preteens, though they can be given to older individuals as well.
HPV is the most common sexually transmitted infection , and most sexually active people will get some type of HPV at some time in their lives, often without realizing it. It's important to have regular health check-ups that include screening for HPV-related diseases, such as cervical cancer, especially for those who are sexually active.
