Delima: Most youths are vitamin D deficient – what to do
The vitamin D grey areas in pediatric primary care.
Very low serum 25-hydroxyvitamin D levels in asymptomatic children living in northeastern Italy
International Journal of Pediatric Endocrinology 2012, 2012:7 doi:10.1186/1687-9856-2012-7
Stefano Mazzoleni ([email protected]) Daniela Toderini ([email protected]) Chiara Boscardin ([email protected])
Article type Letter to the Editor; Submission date 24 March 2012; Acceptance date 18 April 2012; Publication date 18 April 2012
1 MD, Pediatra di Libera Scelta, ULSS 16 Regione Veneto, Padova, Italy
2 MD' Endocrinologa' Medico di Medicina Generale' ULSS 16 Regione Veneto' Padova' Italy
3 MD, Borsista Clinica Pediatrica, Universita di Padova, Padova, Italy
4 MD, Polistudio Pediatrico, via G. D'Annunzio 3/A, I-35028 Piove di Sacco (Padova), Italy
– – – – – – – – – – – –
Italian pediatrician are not supposed to test vitamin D levels – too costly. Upon testing vitamin D levels of patients who did not have “risk factors”, they find most children and all teens were deficient. They are aware that taking 400 or 600 IU, that the govt. recommends will not cure the deficiency. What to do? They may have a concern about getting sued if he prescribes more than the govt. minimum. Wonder if medical cost of being vitamin D deficient exceeds the cost of vitamin D testing.
– – – – – – – – – – – – – – – – – – – – -
The principal questions about the vitamin D topic are far to be resolved: in which children 25-hydroxyvitamin D blood testing is appropriate and how much cholecalciferol should be given in the absence of the test? Analyzing vitamin D status in a group of children cared by a "family pediatrician" in northeastern Italy we noted a high incidence of deficiency in asymptomatic preschool children without risk factors. As routine vitamin D testing is not recommended in the average risk population the supplementation with cholecalciferol represents a "grey area" mostly in pediatric primary care.
Dear Editor,
we read with interest the article by Bener and Hoffmann on the incidence of nutritional rickets in a sun rich country like Qatar [1], where decreased vitamin D was a major risk factor. Hypovitaminosis D is highly prevalent in children throughout the world [2,3] but it is still not clear what is the best practice in pediatric primary care settings. Michael Holick, a recognized expert on the topic, has stated that "there is no need to measure everybody's blood 25-hydroxyvitamin D" [25(OH)D] and that only patients with particular diseases should be screened for vitamin D insufficiency/deficiency [4]. Although the literature has shown that patients with deficiency are much less frequent than those with insufficiency, it is also remarkable that vitamin D deficiency is often subclinical and depending on local situations; for example it may be associated with overweight [5] or underweight [1]. To our knowledge there are only a few studies on children living in northeastern Italy [6-8]: they have been conducted retrospectively [6] or examining patients afferent to a Pediatric Department [7] or asthmatic [8]. On this basis an analysis of vitamin D status was prospectively conducted in children cared by a "family pediatrician" in a rural area near Padua (45° N latitude). In 65 patients the vitamin D test was included in exams ordered for different reasons (suspected anemia, fatigue, poor growth, etc.) between November 2010 and June 2011. Results were retrieved from 58 children (age range 1.1-15.3 years, median age 6.75 years). Serum 25(OH)D was dosed by chemiluminescence; the laboratory normal range was 75-250 nmol/l (30-99 ng/ml); insufficiency was defined as 25-74 nmol/l (10-29 ng/ml), deficiency as < 25 nmol/l (< 10 ng/ml).
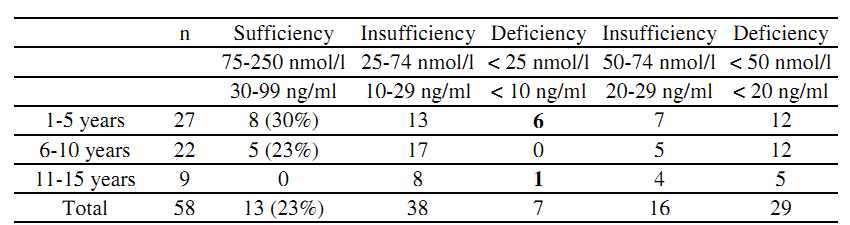
Most of the children (77%) had low serum 25(OH)D levels: 38 of them (66% of all patients) had an insufficiency and 7 (12%) had a deficiency.
Moreover, 29 children (50%) had 25(OH)D < 50 nmol/l (< 20 ng/ml) that is the cut-off recently suggested to diagnose vitamin D deficiency [5,9].
None among the 9 young teens (11-15 years) had a normal value of 25(OH)D and 6 of the 7 children with 25(OH)D < 25 nmol/l (< 10 ng/ml) were between ages 2 and 5 years; this deficiency was asymptomatic in 5/6 cases. Moreover, our children with 25(OH)D > 75 nmol/l (> 30 ng/ml) and those with deficiency didn't differ for exposure to sunlight, food consumption, gender, ethnicity or BMI. Vitamin D status was also irrespective of other blood test results (see Table 1).
Table 1. Vitamin D status of cases based on laboratory reference ranges (white columns) and on recent literature [5,9] (grey columns)
Holick has suggested that "it would be much more cost-effective to implement a vitamin D supplementation program for all children and adults" [4] but the question now is how much vitamin D should be given. If 400 IU cholecalciferol per day may be sufficient in the first year of life [10], much more is needed in older children, assuming that most of them have less or much less than the minimum desirable [11]. Moreover, recommended doses of 600 IU per day [12] probably offer no advantage to children with 25(OH)D < 25 nmol/l (< 10 ng/ml) [13]. Although authoritative guidelines state that routine vitamin D testing is not warranted in the average risk population, the Holick's D-lemma [4] is far from being resolved.
PDF is attached at the bottom of this page
References
Bener A, Hoffmann GF: Nutritional Rickets among Children in a Sun Rich Country. Int JPediatr Endocrinol 2010, 2010:410502. Epub 2010 Oct 27.
Mansbach M, Ginde AA, Camargo CA: Serum 25-Hydroxyvitamin D levels among US children aged 1 to ll years: do children need more vitamin D? Pediatrics 2009, 124:1404-1410.
Rathi N, Rathi A: Vitamin D and child health in the 21st century. Indian Pediatr 2011, 48:619-625.
Holick MF: The D-lemma: To screen or not to screen for 25-Hydroxyvitamin D concentrations. Clin Chem 2010, 56:729-731.
Saintonge S, Bang H, Gerber LM: Implications of a new definition of vitamin D deficiency in a multiracial US adolescent population: the National Health and Nutrition Survey III. Pediatrics 2009, 123:797-803.
Lippi G, Montagnana M, Targher G: Vitamin D deficiency among Italian children [letter]. CMAJ 2007, 177:1529-1530.
Marrone G, Rosso I, Moretti R, Valent F, Romanello C: Is vitamin D status known among children living in Northern Italy? Eur JNutr. 2011 May 4. [Epub ahead of print].
Chinellato I, Piazza M, Sandri M, Peroni D, Piacentini G, Boner AL: Vitamin D serum levels and markers of asthma control in Italian children. J Pediatr 2011, 158:437-441. Epub 2010 Sep 26.
Holick MF, Vitamin D deficiency. N Engl J Med 2007, 357:266-281.
Mutlu GY, Kusdal Y, Ozsu E, Cizmecioglu FM, Hatun S: Prevention of Vitamin D deficiency in infancy: daily 400 IU vitamin D is sufficient. Int J Pediatr Endocrinol 2011, 2011:4. Epub 2011 Jun 28.
Vieth R: Why the minimum desirable serum 25-hydroxyvitamin D level should be 75 nmol/L (30 ng/ml). Best Pract Res Clin Endocrinol Metab. 2011, 25:681-691.
Abrams SA: Dietary Guidelines for Calcium and Vitamin D: A New Era. Pediatrics 2011,127:566-568.
Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ: Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr 2003, 77:204-210.
See also Vitamin D Life
83 percent of children had less than 20 ng of vitamin D – 15 ng avg for hispanic – Aug 2012
96 % of young Koreans had less than 30 ng of vitamin D – March 2012
Vitamin D insufficiency in UK youths – 37X more likely if dark skin – July 2011
Doubling of people less than 30 ng of vitamin D - 75% of whites and 90% of blacks – Feb 2010
Virtually all Chinese teens at 30 degree N have less than 30 ng of vitamin D – Feb 2012
5X increase in vitamin D deficiency after leaving primary school (Tasmania) – Oct 2012
It is much worse in many countries: % of population with less than 20 nanograms