Breast Cancer again associated with low vitamin D – 15th meta-analysis
Vitamin D baseline levels at diagnosis of breast cancer: A systematic review and meta-analysis
Hematol Oncol Stem Cell Ther . 2020 Sep 26;S1658-3876(20)30147-3.
doi: 10.1016/j.hemonc.2020.08.005.
Ioannis A Voutsadakis 1
How many Cancer and Vitamin D meta-analyses will be needed
before there is ANY change by the medical community?
Pages listed in BOTH Breast Cancer AND Meta-analysis
{category}
Colorectal cancer treated by Vitamin D – 19th meta-analysis – Sept 2020
Breast, Prostate and Colon Cancers are still strongly associated with low Vitamin D – Grant Jan 2020
articles are in both Cancer and Meta-analysis categories
articles are in both Prostate Cancer and Meta-analysis categories
- Meta-analysis of Vitamin D lists meta-analyses by type of health problem
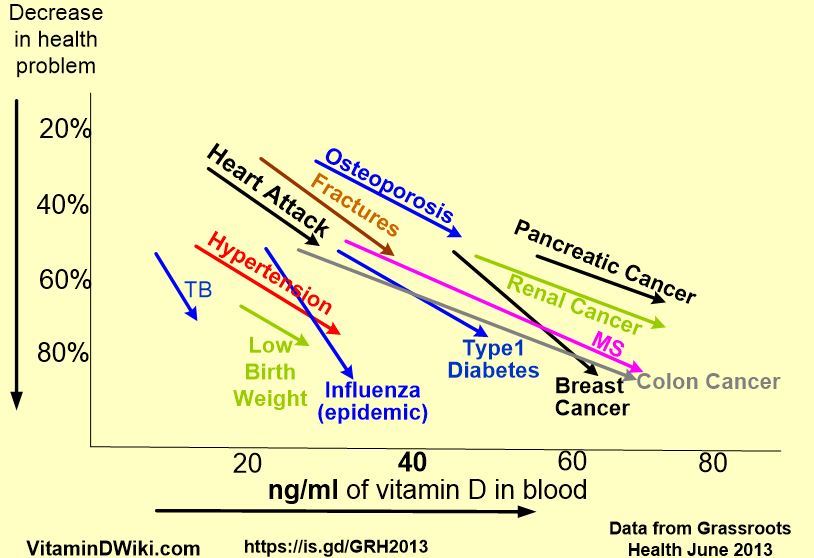
Grassroots Health

Chart of Vitamin D levels vs disease - Grassroots Health June 2013
Background: Vitamin D is a steroid hormone that exerts its actions through ligation of the vitamin D receptor (VDR), a transcription factor of the nuclear receptor family. VDR has not only physiologic actions in calcium metabolism but also several other cellular effects through extensive binding to the DNA and modification of genome expression. In cancer, it has neoplasia-suppressive effects and various mechanisms of action mediating cancer cell inhibition have been described. Vitamin D deficiency has been linked to increased risk of breast cancer. A role of the vitamin once the disease has been diagnosed is also probable.
Methods: A systematic review and meta-analysis of studies that report on vitamin D levels (in the form of its main circulating metabolite, 25-hydroxyvitamin D [25-OHD]) in patients with newly diagnosed breast cancer was performed. Outcomes of interest included the levels of serum 25-OHD in patients with breast cancer, those of matched controlled, in studies that included controls, as well as respective percentages of patients and controls with deficient and insufficient 25-OHD levels.
Results: A total of 25 studies (10 with controls and 15 without controls) provided data on the outcomes of interest. Populations from all continents, besides Australia, were represented in the studies. The mean level of 25-OHD in patients with breast cancer was 26.88 ng/mL (95% CI 22.8-30.96 ng/mL) and the mean level of 25-OHD in control patients was 31.41 ng/mL (95% CI 19.31-43.5 ng/mL). In the patients with breast cancer group, 45.28% (95% CI 24.37%-53.51%) had levels of 25-OHD below 20 ng/mL, whereas this percentage was 33.71% (95% CI 21.61%-45.82%) in controls.
Similarly, 67 .44% (95% CI 48.32%-86.55%) of patients with breast cancer had a baseline level of 25-OHD below 30 ng/mL , whereas this percentage was 33 .71% (95% CI 21.61%-45.82%) in controls.
Conclusion: A high prevalence of vitamin D insufficiency is observed in patients with newly diagnosed breast cancer and may be linked pathophysiologically with breast cancer development or progression. Therapeutic benefits may be provided by manipulation of the vitamin D pathway in breast cancer.
