Bariatric Surgery is Bad for the Bone (reduce vitamin uptake, etc)– 2016
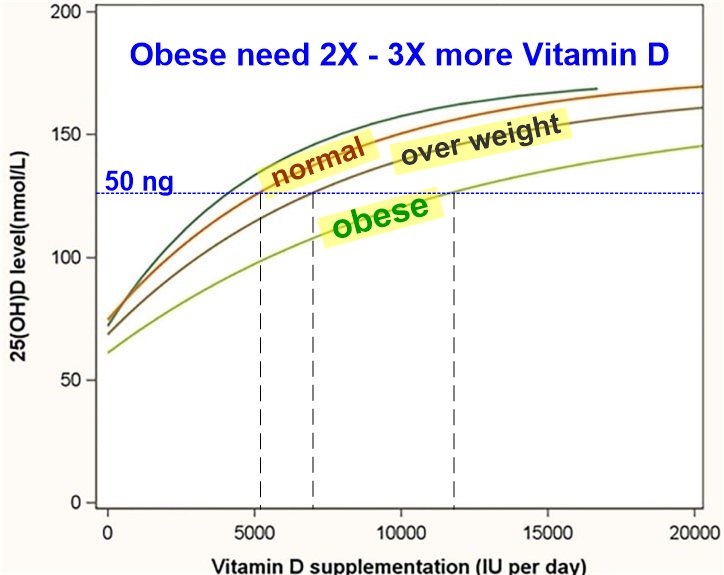 Obese can lose weight with Vitamin D - Bariatric surgery might not be needed* Lost 19 lbs more if add vitamin D to calorie restriction and walking program– July 2018* Obese lost more weight on diet if added 50,000 IU of vitamin D weekly – many RCTsLow Vitamin D before Bariatric Surgery* Vitamin D probably important for Bariatric Surgery – April 2018* Bariatric Surgery problems associated with season, latitude (low Vitamin D) – Dec 2015* Prior to Bariatric Surgery 96 percent were vitamin D deficient – July 2014* Virtually all Bariatric Surgery patients vitamin D deficient – should we routinely supplement – Jan 2011 YES!! After Bariatric Surgery* 50,000 IU of dry vitamin D needed at least daily following obesity surgery – forum Jan 2016 Bio-Tech brand* 11 years after Gastric Bypass Surgery vitamin D still low – Oct 2013* Gastric bypass reduces vitamin D by at least 25 percent – Feb 2011* Overview Deficiency of vitamin D has a chart - a portion of which shows the problems AFTER Bariatric surgery
Obese can lose weight with Vitamin D - Bariatric surgery might not be needed* Lost 19 lbs more if add vitamin D to calorie restriction and walking program– July 2018* Obese lost more weight on diet if added 50,000 IU of vitamin D weekly – many RCTsLow Vitamin D before Bariatric Surgery* Vitamin D probably important for Bariatric Surgery – April 2018* Bariatric Surgery problems associated with season, latitude (low Vitamin D) – Dec 2015* Prior to Bariatric Surgery 96 percent were vitamin D deficient – July 2014* Virtually all Bariatric Surgery patients vitamin D deficient – should we routinely supplement – Jan 2011 YES!! After Bariatric Surgery* 50,000 IU of dry vitamin D needed at least daily following obesity surgery – forum Jan 2016 Bio-Tech brand* 11 years after Gastric Bypass Surgery vitamin D still low – Oct 2013* Gastric bypass reduces vitamin D by at least 25 percent – Feb 2011* Overview Deficiency of vitamin D has a chart - a portion of which shows the problems AFTER Bariatric surgery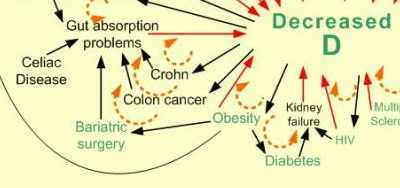
Bariatric Surgery: Bad to the Bone, Part 1.
Integr Med (Encinitas). 2016 Mar;15(1):48-54.
Pizzorno L is senior medical editor at Integrative Medicine Advisers, LLC, in Seattle, Washington.
📄 Download the PDF from Vitamin D Life
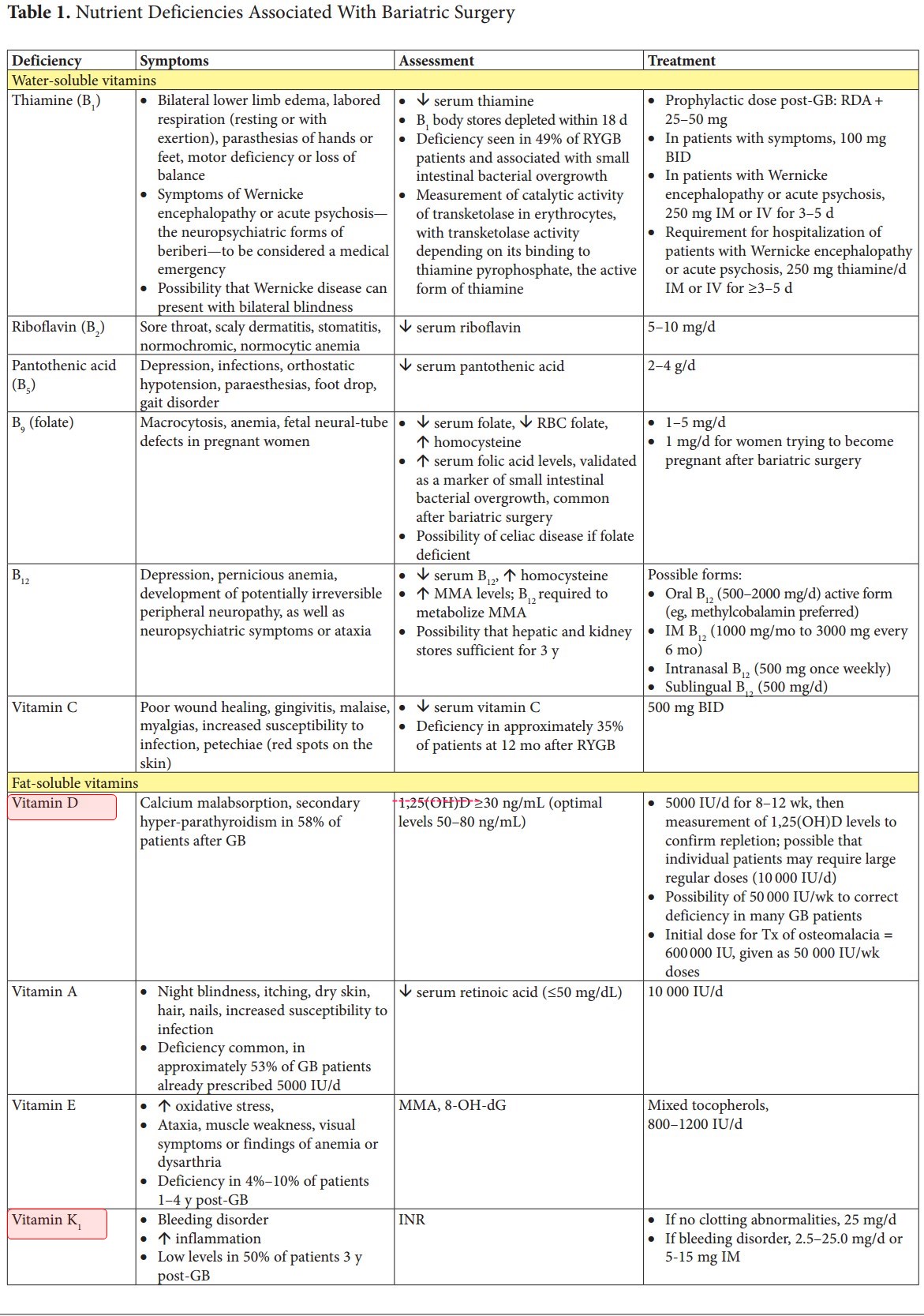
Obesity is now a global epidemic affecting a significant and rapidly increasing number of adults, adolescents, and children. As the incidence of obesity has increased, so has the use of bariatric surgery as a medical solution. A growing number of studies now report that, despite calcium and vitamin D supplementation, the most frequently performed types of bariatric surgery, the Roux-en-Y gastric bypass and the sleeve gastrectomy, cause significant ongoing bone loss. In resources available to the general public and to physicians, this adverse outcome is rarely mentioned or is attributed solely to reduced calcium absorption. Recent studies investigating micronutrient malabsorption and changes in a wide range of hormones induced by bariatric surgery now indicate that calcium malabsorption is the tip of a formidable iceberg. The current article, part 1 of a 2-part series, reviews the latest research findings confirming that obesity prevalence is skyrocketing and that bariatric surgery causes ongoing, accelerated bone loss. Part 1 also discusses the mechanisms through which the bariatric surgery-induced malabsorption of key nutrients adversely affects bone homeostasis. Part 2 discusses the specific changes seen in bone metabolism after bariatric surgery and reviews current data on the underlying mechanisms, in addition to nutrient malabsorption, which are thought to contribute to bariatric surgery-induced ongoing accelerated bone loss. These processes include mechanical unloading and changes in a wide variety of hormones (eg, leptin, adiponectin, testosterone, estradiol, serotonin, ghrelin, glucagon-like peptide 1, and gastric inhibitory peptide). Also, part 2 covers interventions that may help lessen bariatric surgery-induced bone loss, which are now beginning to appear in the medical literature. Bariatric surgery's adverse effects on bone must be widely recognized and protocols developed to prevent early onset osteoporosis in the recipients of an increasingly utilized and otherwise potentially life-saving surgery.
Bariatric Surgery: Bad to the Bone, Part 2.
Integr Med (Encinitas). 2016 Apr;15(2):35-46.
Pizzorno L1.
Lara Pizzorno, md iv, ma , lmt , is senior medical editor at Integrative Medicine Advisers, LLC, in Seattle, Washington.
📄 Download the PDF from Vitamin D Life
As discussed in Part 1, obesity is now a global epidemic affecting a significant and rapidly increasing number of adults, adolescents, and children. As the incidence of obesity has increased, so has the use of bariatric surgery to treat it. A growing number of recently published studies have reported that, despite calcium and vitamin D supplementation, the most frequently performed types of bariatric surgery, the Roux-en-Y gastric bypass (RYGB) and the sleeve gastrectomy (SG), cause significant, ongoing bone loss. Recent studies investigating nutrient malabsorption and changes in a wide range of hormones that are induced by bariatric surgery have indicated that calcium malabsorption is just the tip of a formidable iceberg.
Part 1 reviewed the latest research findings confirming that the prevalence of obesity is, in fact, skyrocketing and that bariatric surgery causes ongoing accelerated bone loss. Part 1 also discussed the mechanisms through which the malabsorption of key nutrients induced by bariatric surgery adversely affects bone.
The current article, Part 2, reviews the specific changes seen in bone metabolism after bariatric surgery and the current data on the underlying mechanisms, in addition to nutrient malabsorption, that may contribute to bariatric surgery-induced bone loss.
These mechanisms include
mechanical unloading,
calcium malabsorption despite maintenance of vitamin D levels of ≥30 ng/mL, and
changes in a number of hormones, including leptin, adiponectin, testosterone, estradiol, serotonin, ghrelin, glucagon-like peptide 1 (GLP-1), and gastric inhibitory peptide (GIP).
Research discussing the use of nutritional supplements to help ameliorate bariatric surgery-induced bone loss is summarized. The adverse effects of bariatric surgery on bone must be widely recognized, and protocols must be developed to prevent early onset osteoporosis in recipients of this increasingly utilized and otherwise potentially life-saving surgery.
